The HUC will interact with a wide variety of physicians in the hospital environment during the course of their daily duties. They will also be expected to enter correct physician data into the patient record and contact the appropriate physician for referrals, consults, and patient care-related issues. Therefore, it is important that they have a good understanding of the most common types of physicians in the hospital, and their scope of practice.
General Terms Related to Hospital Physicians
Working in a hospital, the HUC will hear several terms related to physicians based upon where they are in their training, clinical role in care of the patient, or even the time of day. Below are some common general terms that may be used to describe physicians of any specialty within the hospital environment.
Attending Physicians/Most Responsible Physicians (MRPs): These physicians have completed their residency and are certified in their chosen specialty. They make the primary decisions when it comes to patient care and supervise the work of medical students, residents, and interns. The MRP is typically a surgeon, medical specialist, or hospitalist. Only one doctor may be MRP for a patient at one time, although the MRP may change throughout a hospital admission.
Consultant: These doctors provide opinions or recommendations on patient conditions outside the MRP’s area of expertise at their request. Some common consults may include cardiology or anaesthesia consultations prior to proposed surgical procedures.
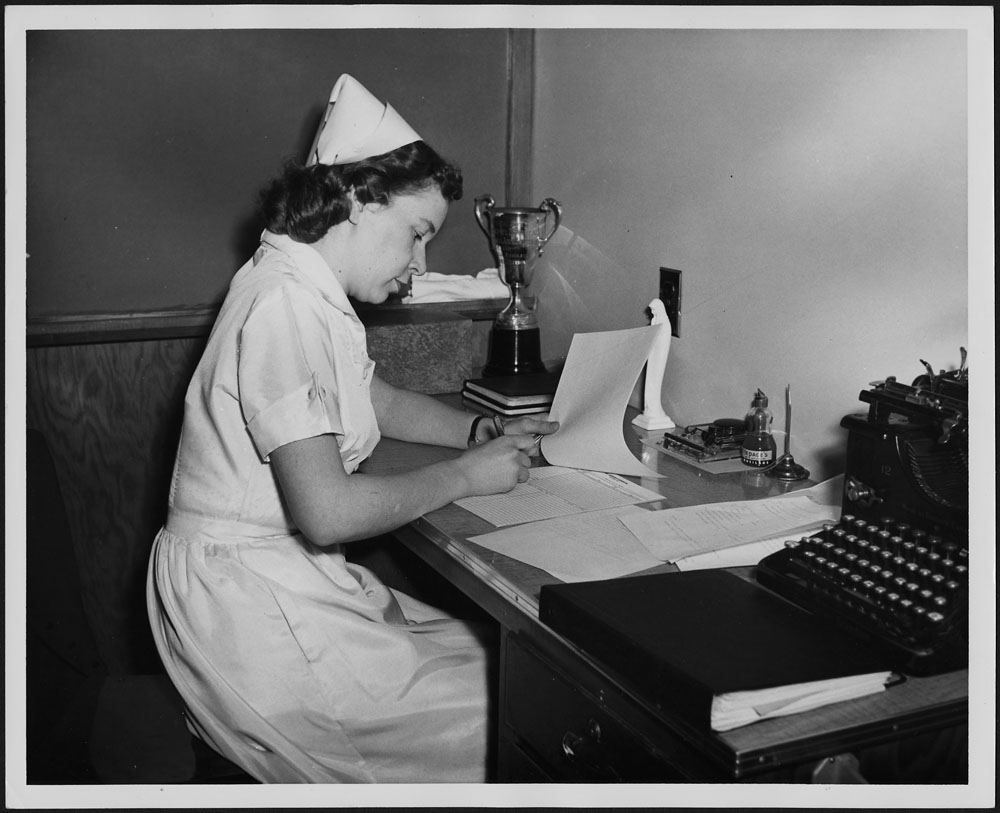
Doctors On-Call/On-Call Physicians: In addition to their own practice, these doctors work on weekends, evenings, and other shifts to answer questions or cover emergencies. On-call duties are typically divided evenly amongst a specialty type; for example, general surgeons, so that one of them is always available after hours.
Interns: These doctors have completed medical school and are in their first year of residency.
Residents: These doctors have graduated medical school and are continuing their training for two to seven years in a specific medical area, like family medicine or surgery. Residents provide direct care, under the supervision of a fully credentialed attending physician who approves their decisions.
Specialists and Subspecialists
There are a number of different specialties that a physician can complete, and they may change specialties during their career. Some of the more common specialties are described below, along with reasons why a patient might be referred to them.
Anaesthesiologists: These doctors work mostly with patients undergoing surgery. They use their knowledge of pharmacy and physiology to ensure that patients remain unconscious or with no sensation during their surgical procedures. Anaesthesiologists may also be consulted to help with pain management in patients with pain problems outside the operating room, such as administering epidurals during labour and post-operative pain management.
Cardiologists: These medical doctors specialize in diagnosing and treating heart disease. They do not perform surgery but treat common cardiac issues such as arrhythmias, congestive heart failure, and other cardiac pathologies.
Cardiovascular Surgeons: These doctors perform surgical treatments for the heart and other thoracic organs. They do not provide ongoing care as cardiologists do, but they complete the required patient assessments, surgical procedures, and immediate aftercare.
Emergentologists/Emergency Medicine: These doctors work in emergency departments to provide care to acutely ill or injured patients. Their patients can present with a variety of different pathologies and injuries.
Endocrinologists: These doctors specialize in the treatment of endocrine system disorders that affect hormone levels and may treat patients who have either high or low levels of certain hormones, such as diabetes and growth problems.
Gastroenterologists: These doctors specialize in the diagnosis and medical treatment of conditions affecting the digestive system. They may treat patients with an array of digestive pathologies that could include gastroesophageal reflux disease (GERD), Crohn’s disease, and ulcerative colitis.
General Surgeons: These doctors perform surgical procedures on many organs and bodily systems, including the gastrointestinal system, the endocrine system, the breasts, and the skin (Berry, 2019).
Geriatric Medicine Physicians/Geriatricians: These internal medicine or family medicine doctors treat older patients, often over 75 years of age, for any medical needs and assessments they may require.
Hematologists: These doctors specialize in diagnosing and treating blood disorders. They are very knowledgeable about different blood conditions and laboratory procedures. A patient could be referred to this physician if they have a blood disorder related to clotting, anemia, hemophilia, or other blood-related factors.
Hospitalists: These doctors specialize in primary care for hospitalized patients. These doctors cover the gap in primary care that occurs during hospitalization by assuming the primary care role during the hospitalization period. Hospitalists may be family physicians or Internists.
Infectious Disease Doctors: These doctors specialize in diseases and conditions that are contagious or difficult to diagnose, such as nosocomial infections, TB, influenza, or cellulitis. This specialist can assist with the diagnosis, treatment, and ways of decreasing the spread of an illness.
Intensivists: These doctors, often internists with advanced training, work in intensive care units treating critically ill patients. May also be called critical care physicians (Santiago, 2023).
Internal Medicine Physicians/Internists: These doctors specialize in medically treating disorders with the internal organs and systems of the body for adults. May be general internists or specialize in a subspecialty (WebMD Editorial Contributors, 2023).
Neonatologists: These doctors are pediatricians with specialty training in the care of premature and critically ill newborns (Nemours KidsHealth, 2022).
Nephrologists: These doctors specialize in diagnosing and medically treating kidney diseases. They treat patients with kidney failure and other pathologies that relate to the kidneys.
Neurologists: These doctors specialize in the prevention, diagnosis, and medical treatment of disorders and conditions related to the brain, spinal cord, nerves, and muscles. They may treat pathologies such as multiple sclerosis, epilepsy, tremors, cerebral palsy, Alzheimer’s disease, and Parkinson’s disease.
Obstetrician/Gynecologists (OB/GYNs): Obstetricians provide care to the mother and fetus through pregnancy and labour, and to the mother during the postpartum period. Gynecologists focus on the diagnosis, treatment, management, and prevention of diseases and disorders of the female reproductive system. A patient may see a gynecologist if they have conditions such as pelvic inflammatory disease, endometriosis, or other pathologies that affect the female reproductive system. OB/GYNs provide both obstetric and gynecology services to patients.
Oncologists: These doctors specialize in diagnosing and treating patients who have cancer and malignancies in any area of the body.
Ophthalmologists: These doctors specialize in screening, diagnosing, and managing the care of patients with optical, medical, and surgical diseases or disorders of the eye, such as cataracts or detached retinas.
Orthopedic Surgeons: These doctors specialize in the prevention, diagnosis, treatment, and surgery of disorders and diseases related to the musculoskeletal system. They may treat patients who have injuries to their musculoskeletal system from trauma or from complications of aging or repetitive use.
Otolaryngologists (ENTs): These doctors specialize in the treatment of conditions in the ears, nose, and throat. They may see patients with hearing difficulties, difficulty swallowing, issues with balance, or tinnitus.
Palliative Medicine Specialists: These doctors help patients who have serious illnesses or are at the end of life by focusing on managing pain and improving quality of life.
Pathologists: These doctors specialize in the study aspects of disease. They often work in the lab, studying tissue, blood, and body fluid samples from patients and working to assist in the diagnosis and prognosis of disease and illness.
Pediatricians: These doctors provide ongoing care to children, for any medical needs they may have. These doctors can provide both long-term and acute care, and children can be referred to them from family physicians if they require more specialized care.
Plastic Surgeons: These doctors specialize in medically necessary reconstructive and cosmetic procedures and/or surgeries which modify a person’s appearance (Santiago, 2023).
Psychiatrists: These medical doctors specialize in providing treatment for diseases of the mind. They complete comprehensive assessments and diagnose and plan care for patients who are experiencing various forms of mental illness and emotional and behavioural disorders.
Pulmonologists/Respirologists: These medical doctors specialize in the diagnosis and treatment of diseases related to the respiratory system. Patients may see this specialist if they have asthma, chronic obstructive pulmonary disease (COPD), emphysema, or other respiratory signs or symptoms.
Radiologists: These doctors specialize in using medical imaging techniques such as X-rays, CT scans or MRIs in the study, diagnosis, and treatment of disease. Their role is often as a consultant to other physicians for patients who require diagnostic imaging.
Rheumatologists: These doctors specialize in medically treating systemic diseases that affect the joints and muscles, including autoimmune disorders that affect multiple body systems, as well as rheumatoid arthritis, lupus, and psoriasis.
Urologists: These doctors specialize in the diagnosis and treatment of urinary and male genitourinary system conditions, disorders, and diseases such as prostate disease and renal and bladder dysfunctions. In addition to diagnosis and medical treatment, they may also perform surgical repair. Common patient conditions that they treat include kidney stones, kidney failure, benign prostatic hyperplasia, and bladder dysfunction. It is important to note that this specialist provides care and assessment for both male and female urinary systems.
Vascular Surgeons: These doctors specialize in treating diseases of the blood and lymphatic vessels. They repair and replace diseased or damaged vessels, remove plaque from vessels, insert venous catheters, and perform traditional surgery.
References
Berry, J. (2019, December 16). Types of doctors and what they do. Medical News Today.
Nemurs Kid’s Health. (2022). Doctors and hospitals.
Santiago, A.(2023, November 4). Common types of doctors and what they do. verywell health.
WebMD Editorial Contributors. (2023, July 15). What is an internist? WebMD.
Attributions










 of a person, you would round up to
of a person, you would round up to  RNs.
RNs.