- Identify the anatomy of the heart
- Describe the main functions of the heart
- Spell the heart medical terms and use correct abbreviations
- Identify the medical specialties associated with the heart
- Explore common diseases, disorders, and procedures related to the heart
Cardiovascular System – Heart Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the cardiovascular system – Heart.
An interactive or media element has been excluded from this version of the text. You can view it online here:
https://ecampusontario.pressbooks.pub/medicalterminology/?p=259
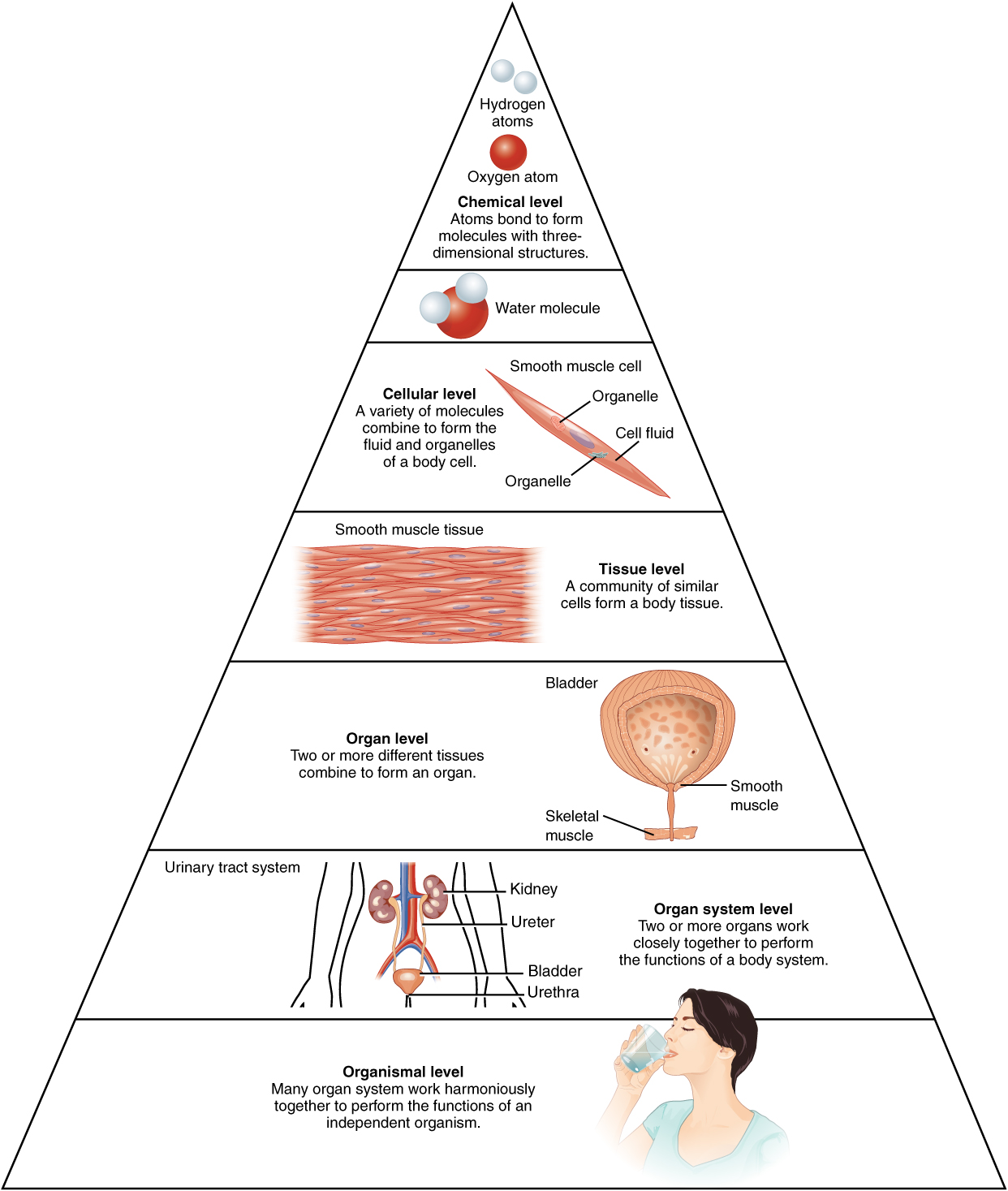
Introduction to the Heart
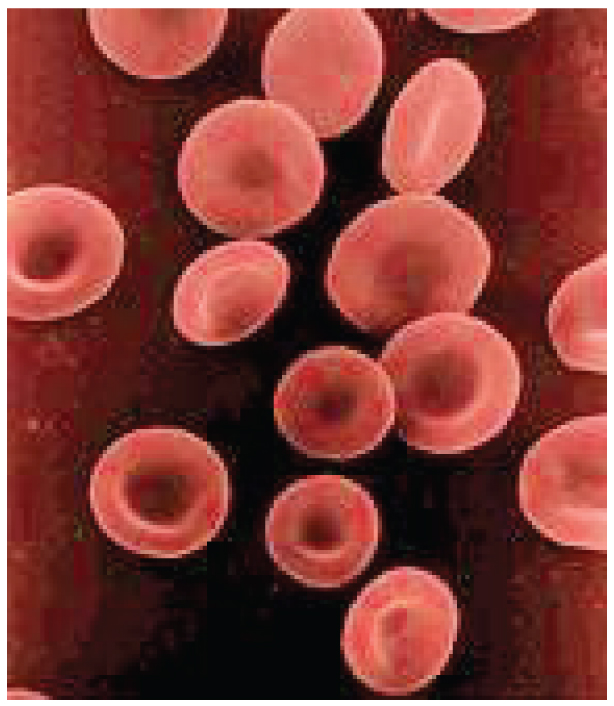
The heart is a fist-sized vital organ that has one job: to pump blood. If one assumes an average heart rate of 75 beats per minute, a human heart would beat approximately 108,000 times in one day, more than 39 million times in one year, and nearly 3 billion times during a 75-year lifespan. At rest, each of the major pumping chambers of the heart ejects approximately 70 mL blood per contraction in an adult. This would be equal to 5.25 liters of blood per minute and approximately 14,000 liters per day. Over one year, that would equal 10,000,000 liters of blood sent through roughly 100,000 km of blood vessels. In order to understand how that happens, it is necessary to understand the anatomy and physiology of the heart.
Watch this video:

A YouTube element has been excluded from this version of the text. You can view it online here: https://ecampusontario.pressbooks.pub/medicalterminology/?p=259
Media 12.1. The Heart, Part 1 – Under Pressure: Crash Course A&P #25 [Online video]. Copyright 2015 by CrashCourse.
Cardiovascular System – Heart Medical Terms
An interactive or media element has been excluded from this version of the text. You can view it online here:
https://ecampusontario.pressbooks.pub/medicalterminology/?p=259
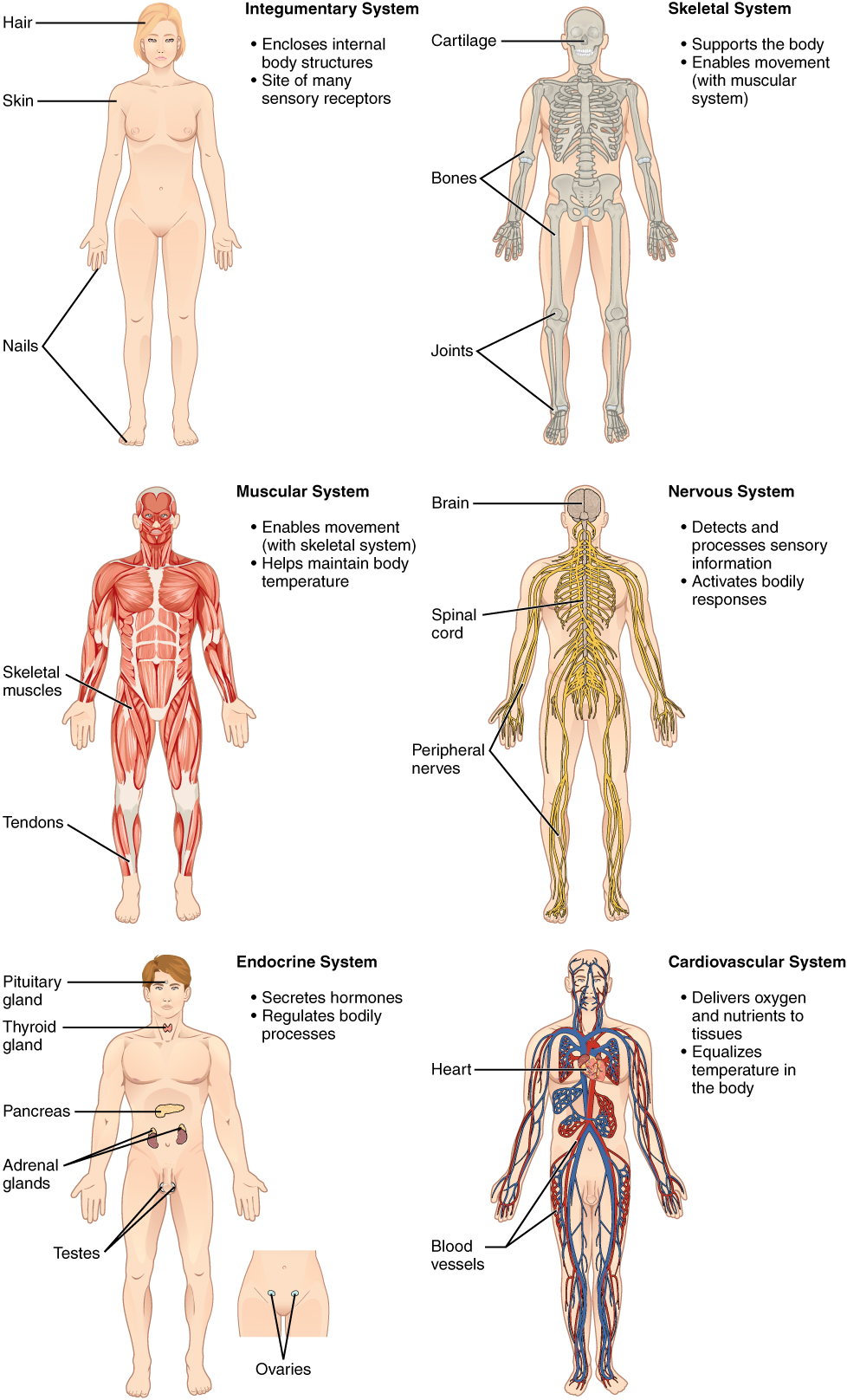
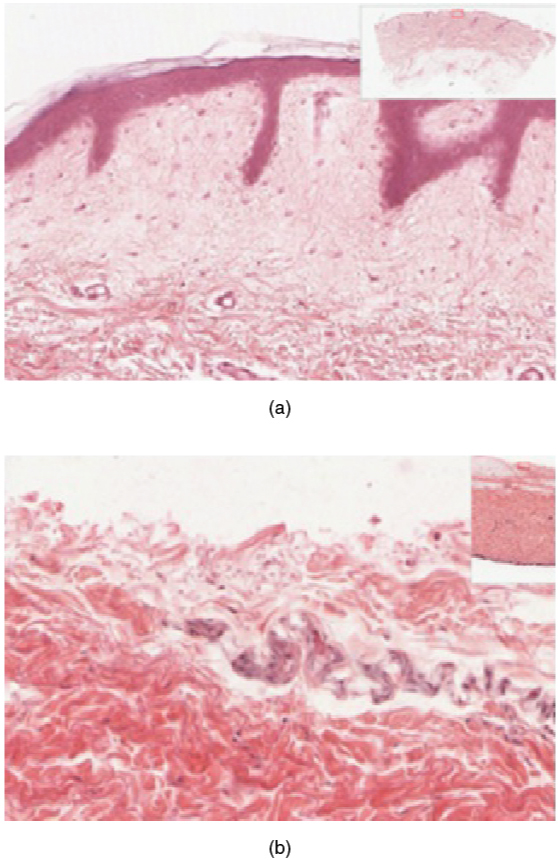
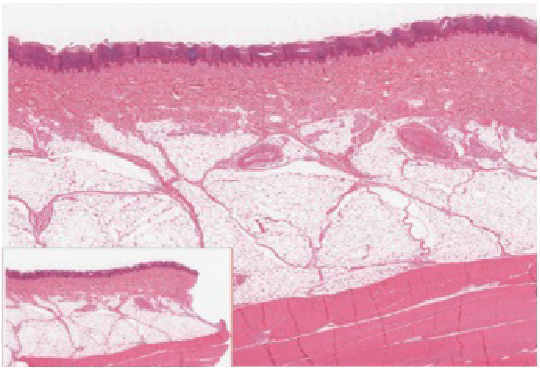
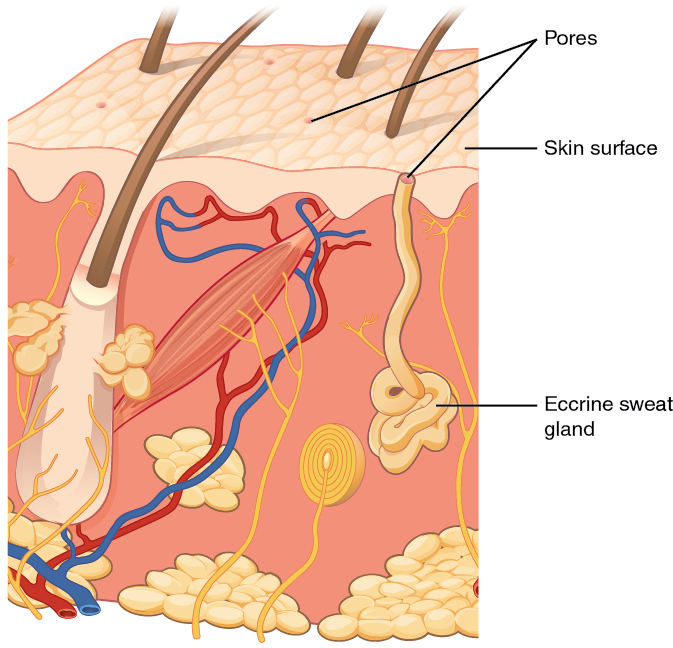
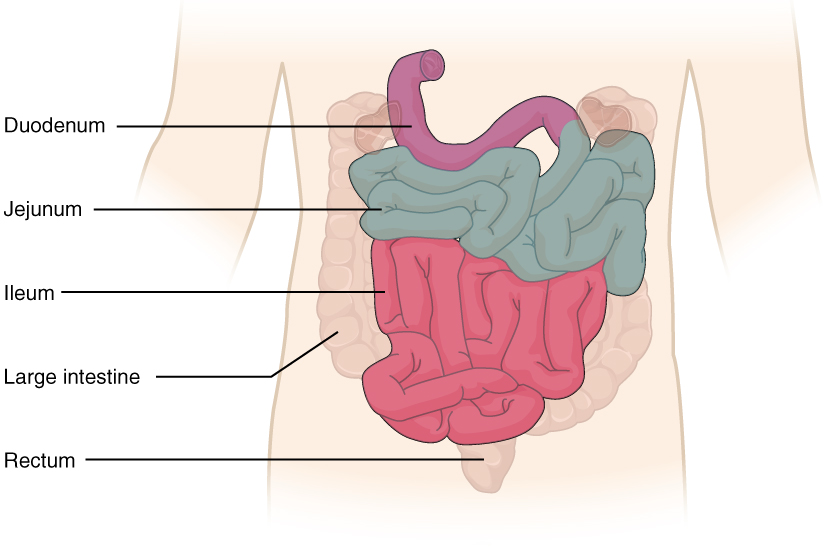
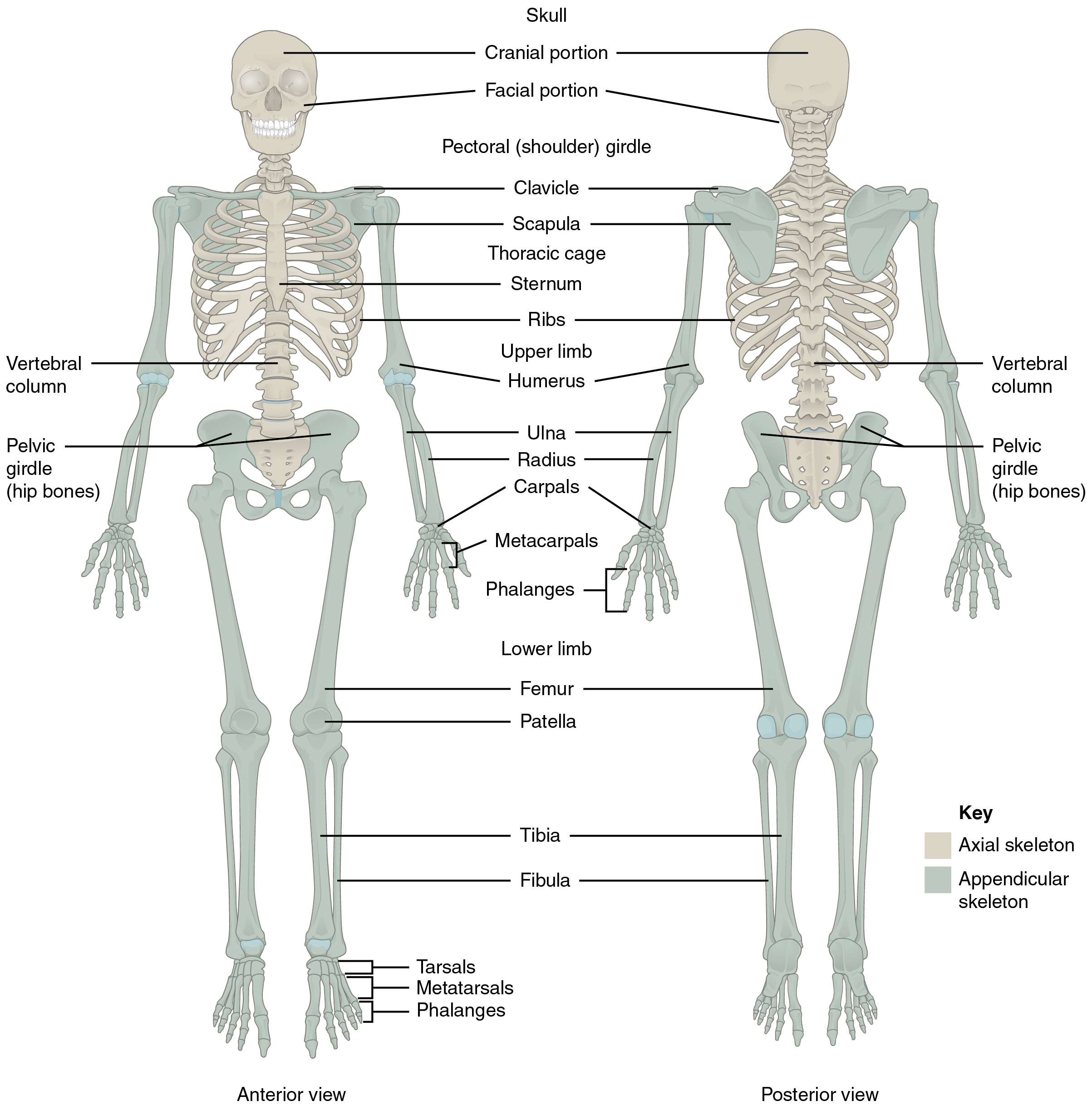
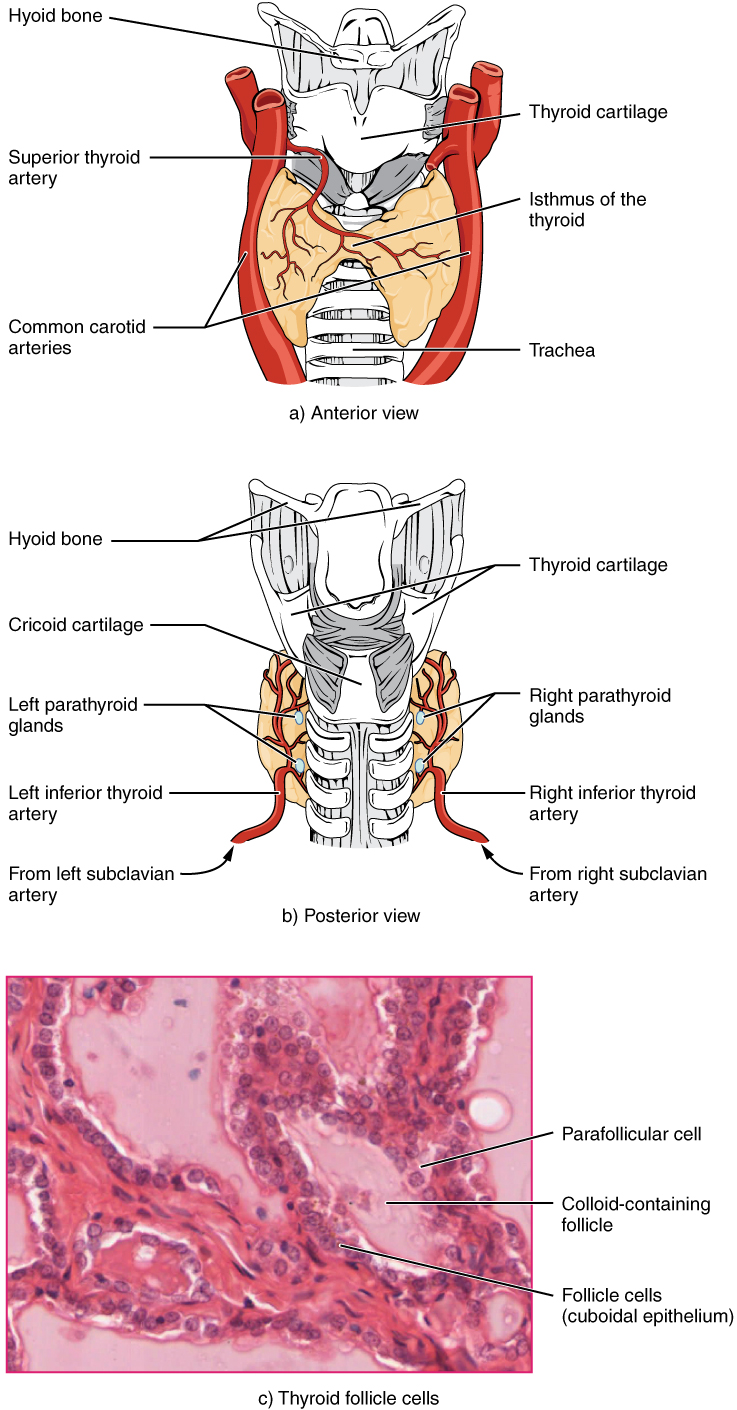
Anatomy of the Heart
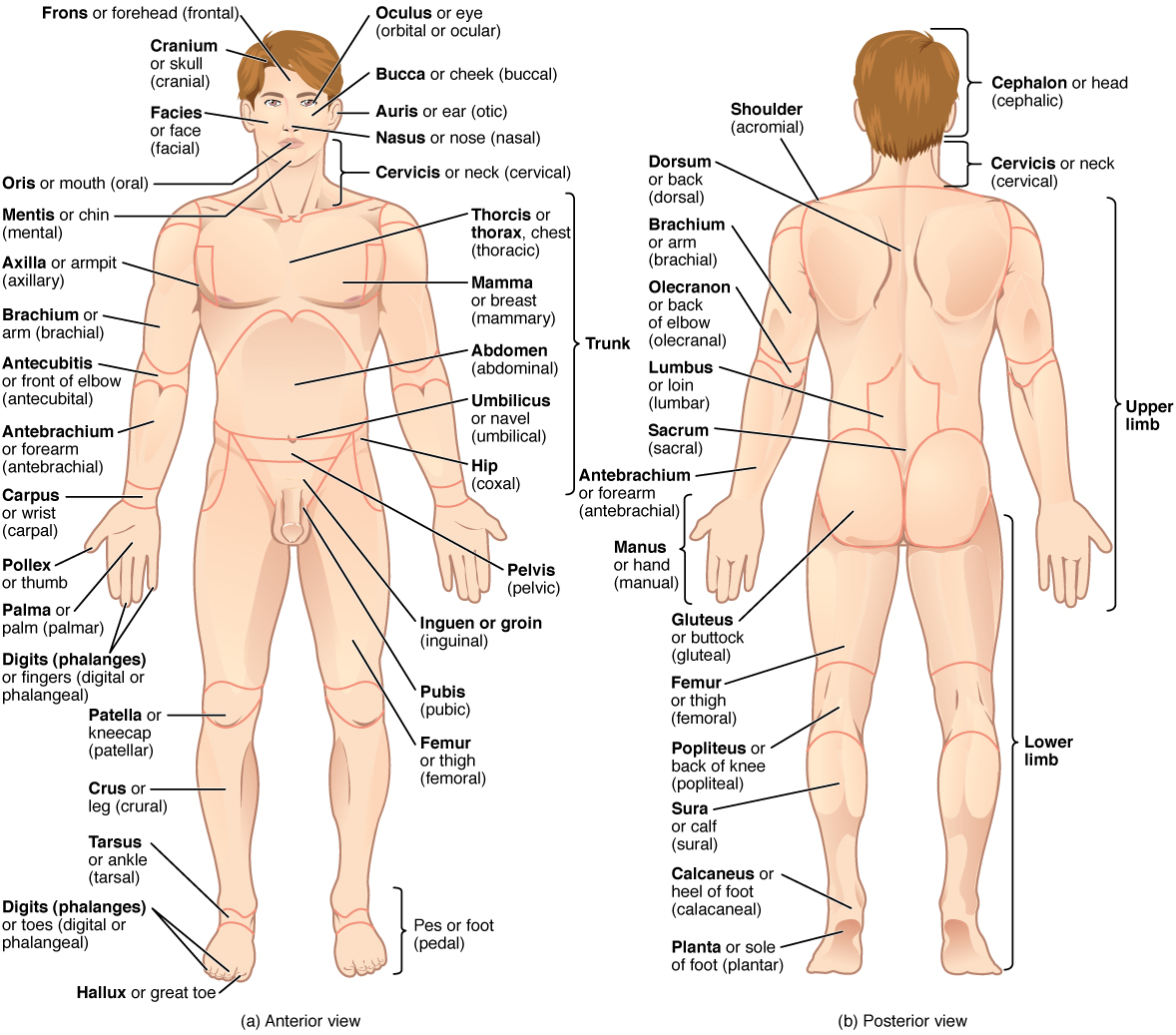
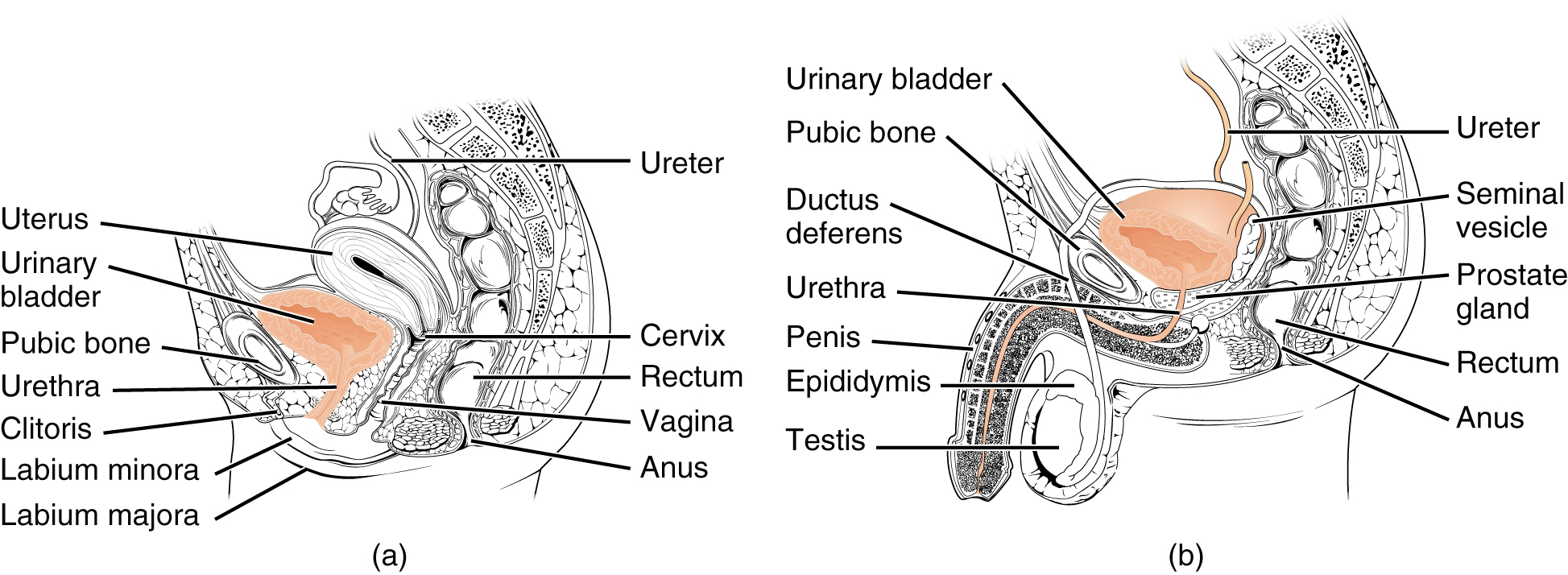
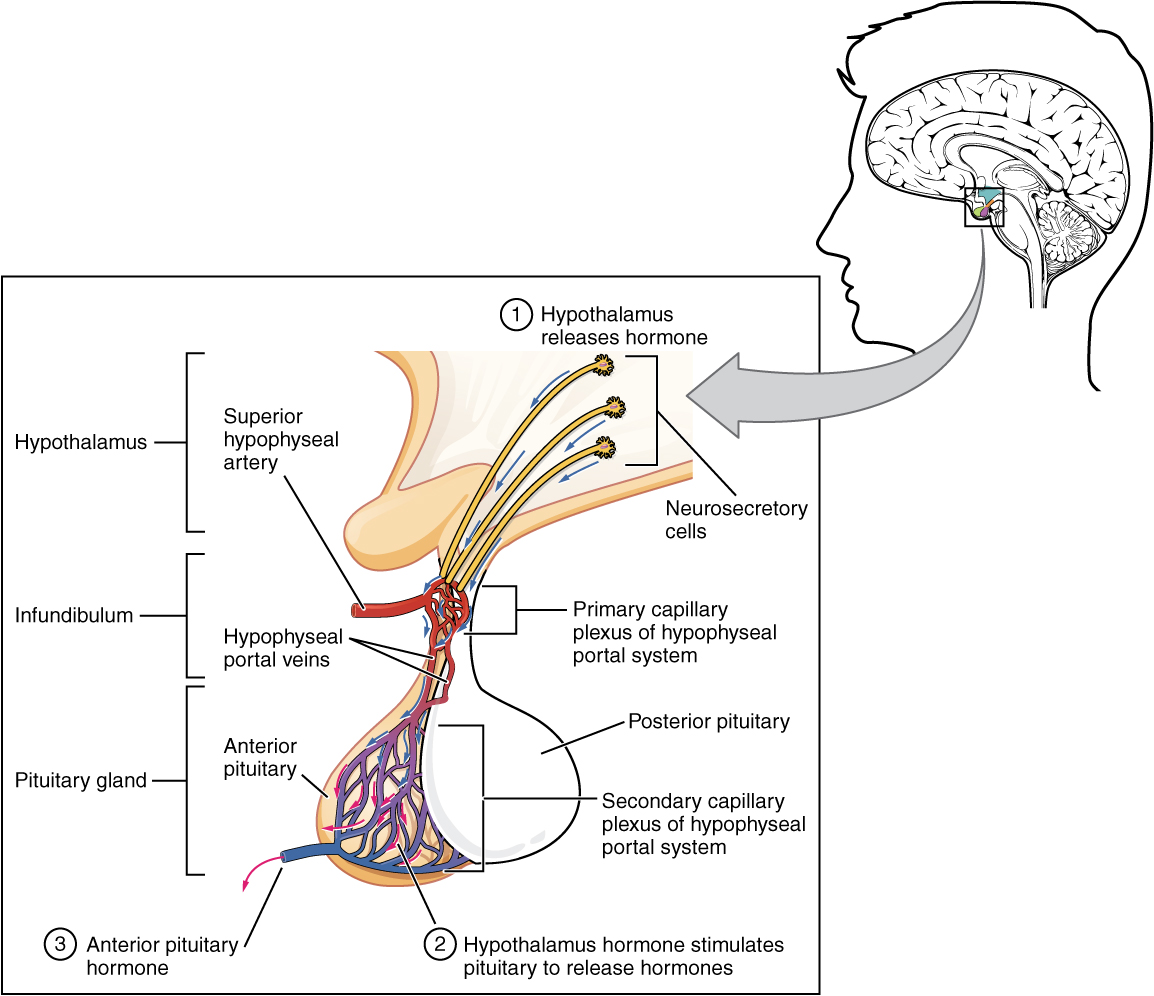
Location
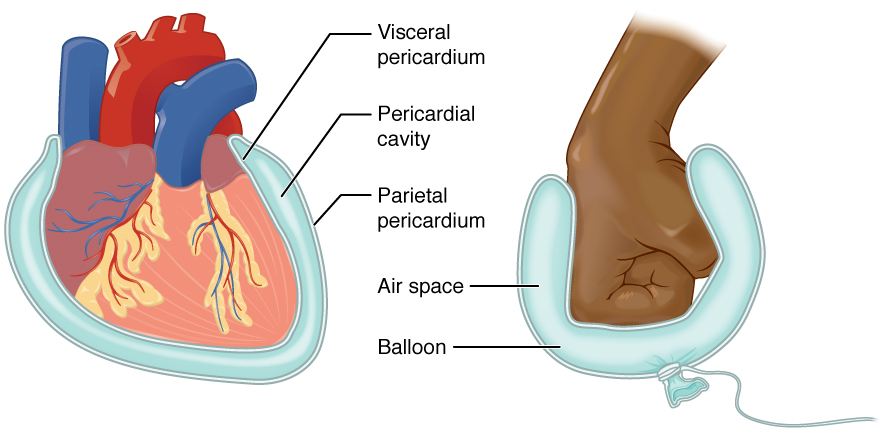
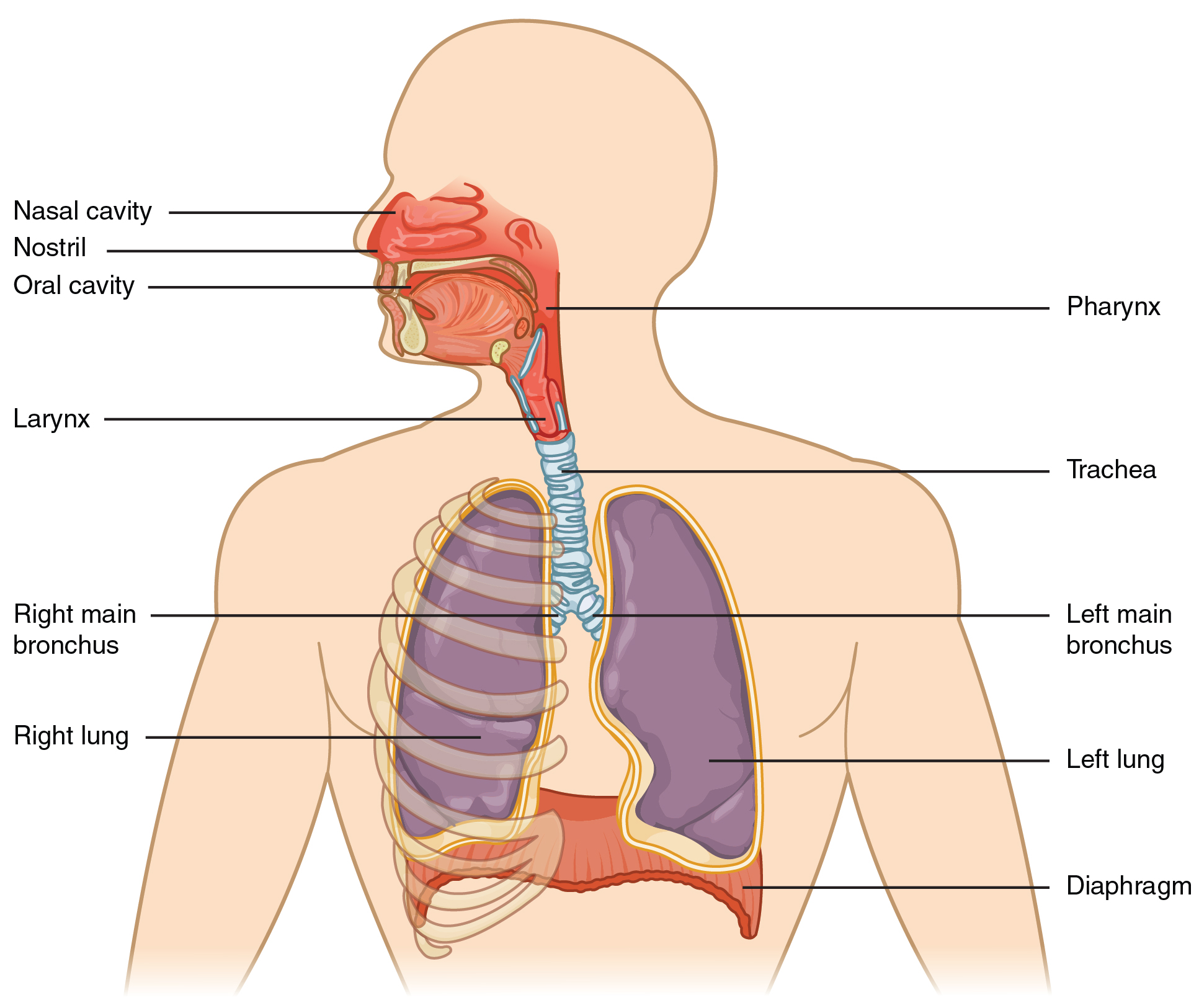
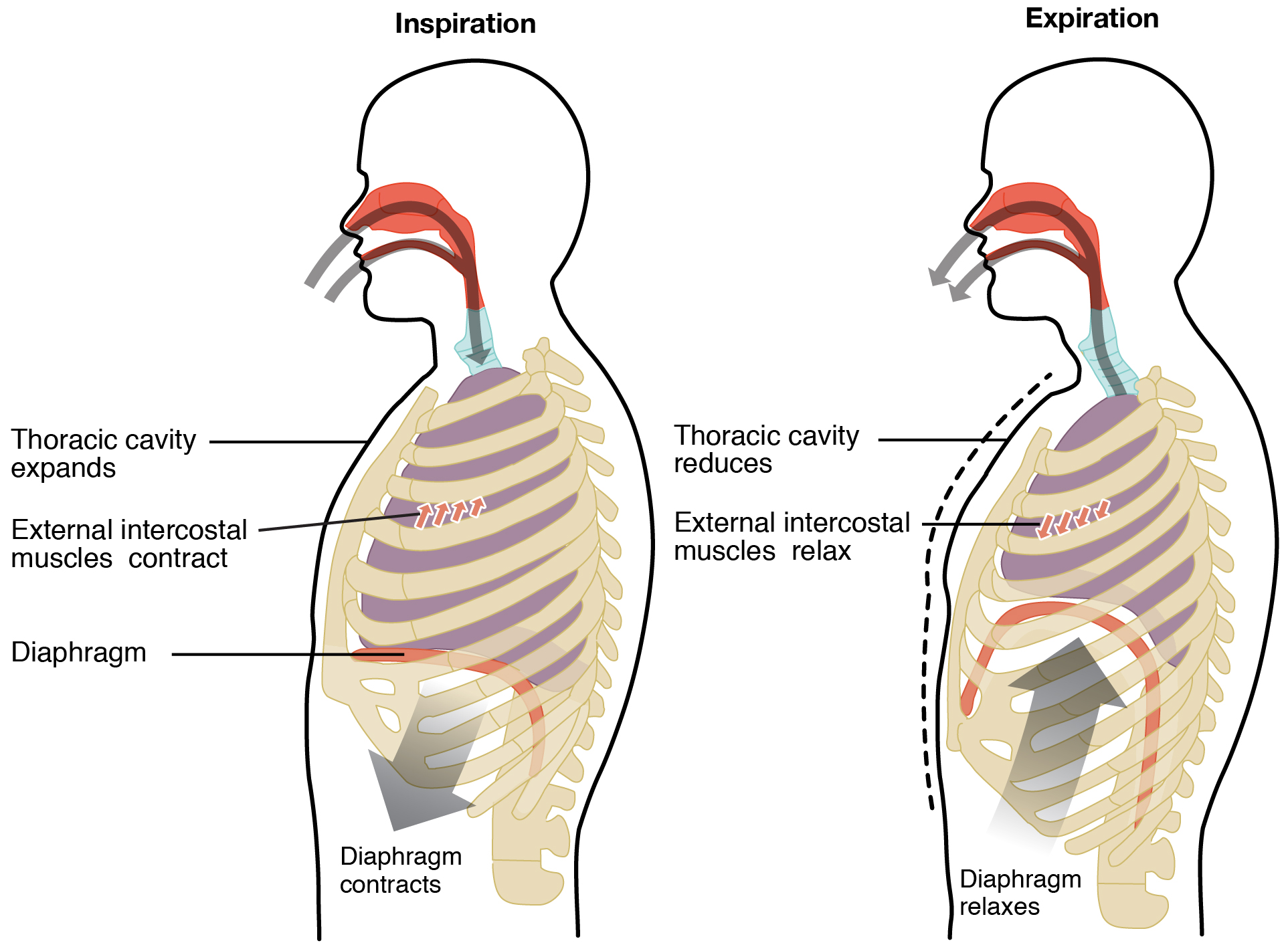
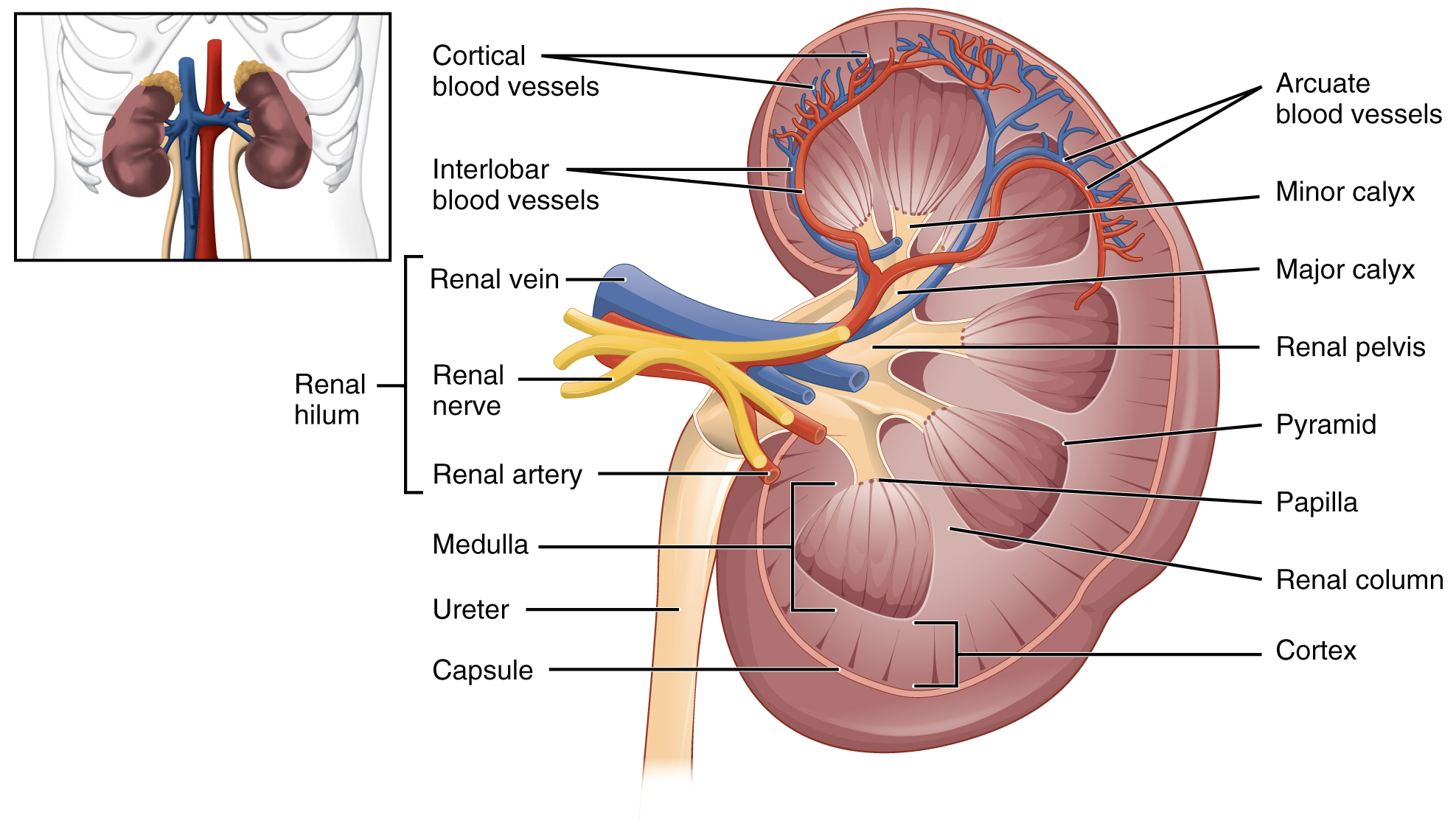
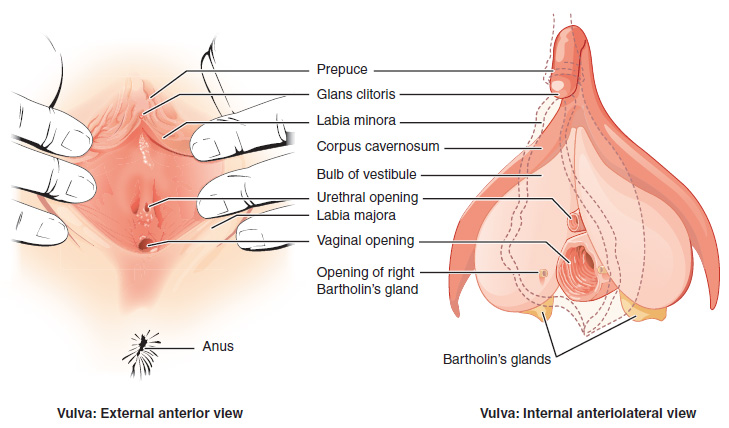
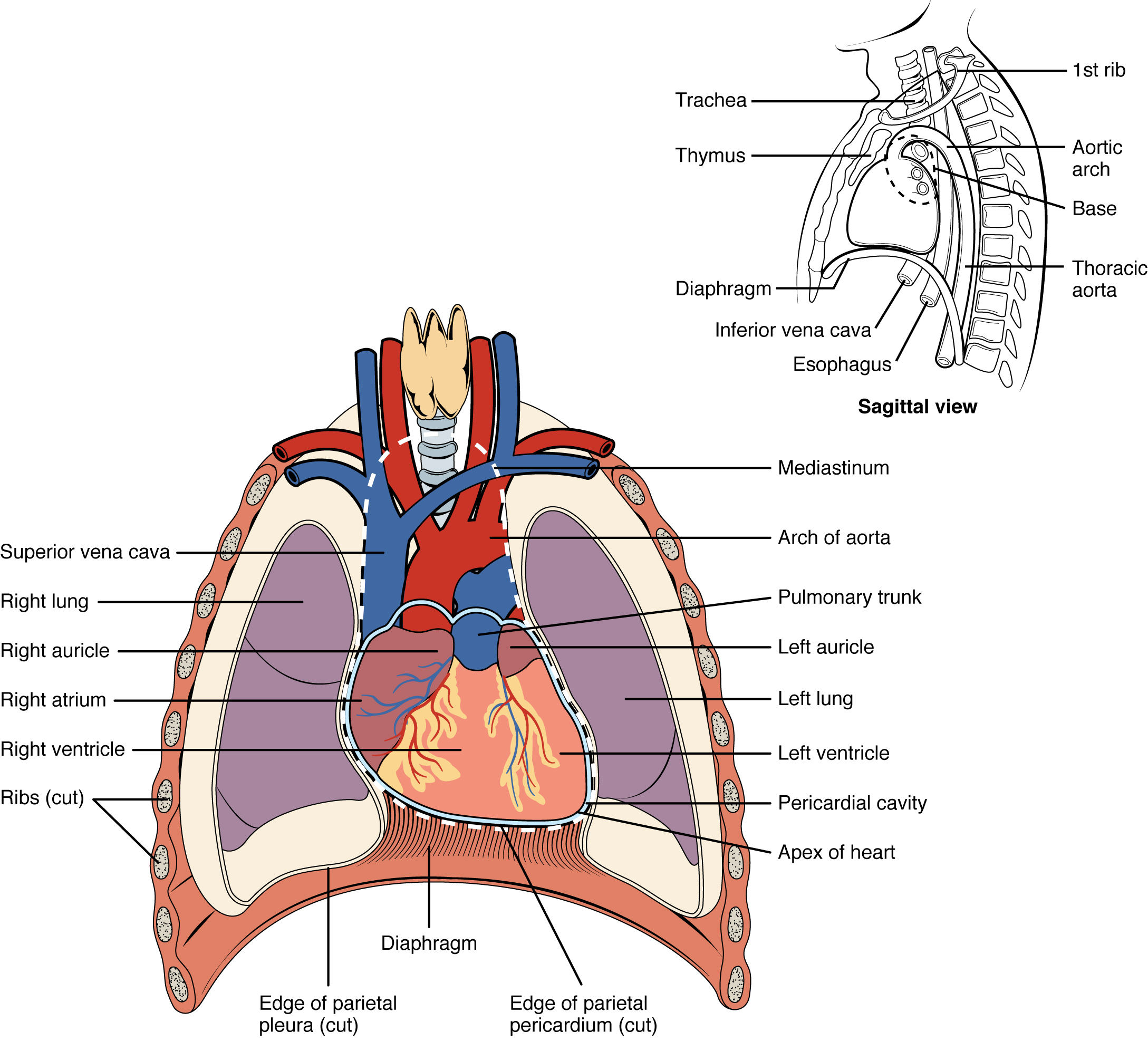
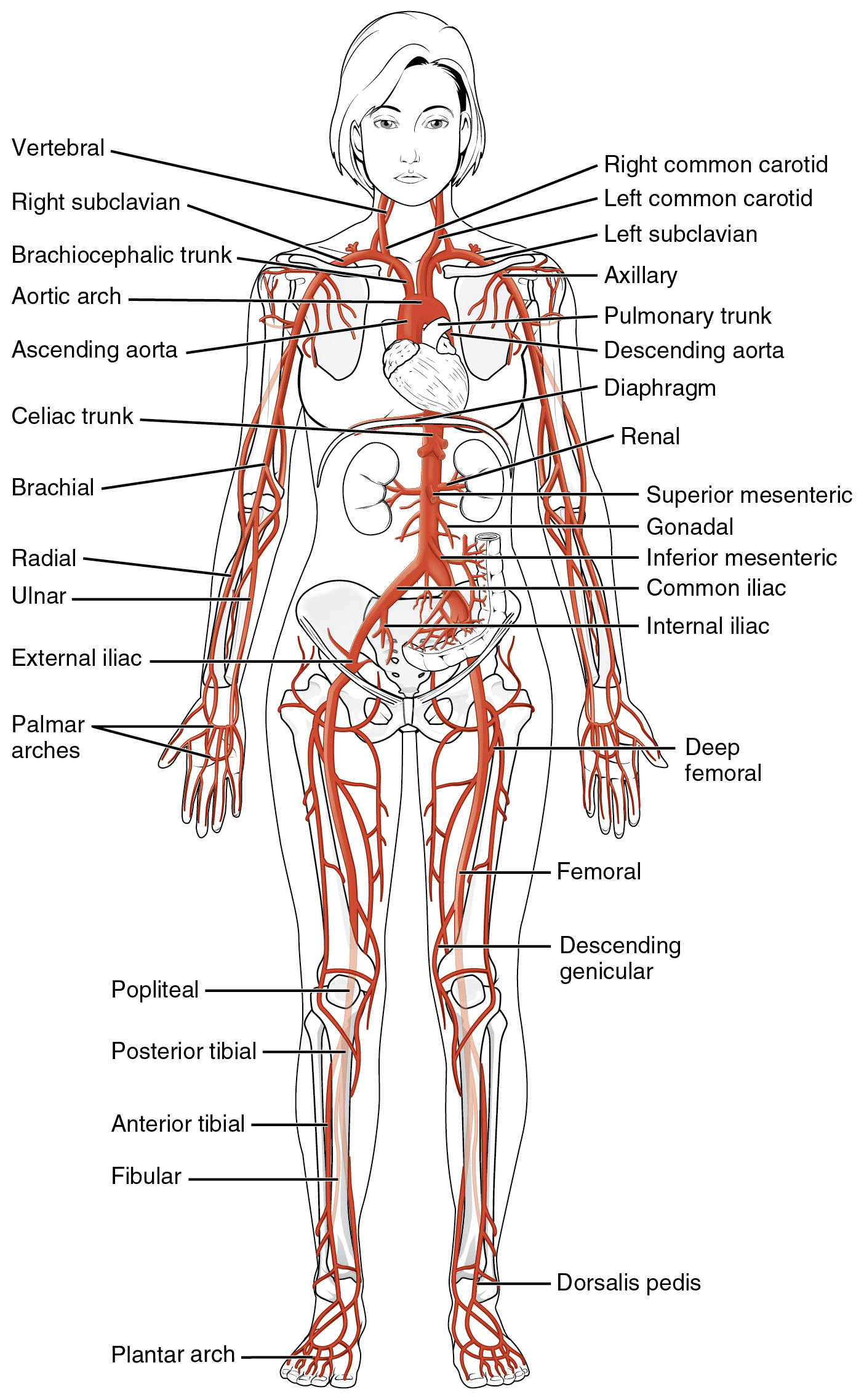
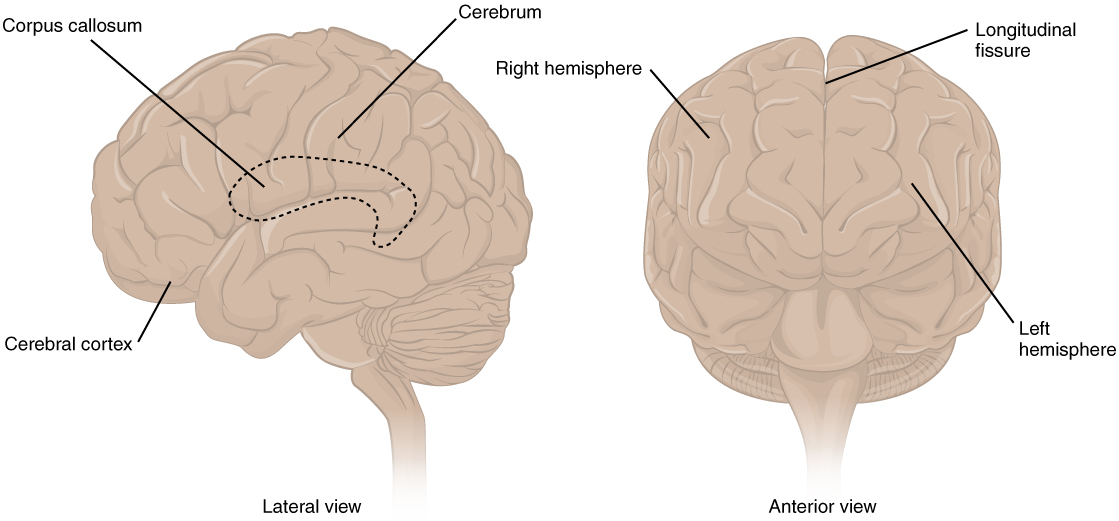
The human heart is located within the thoracic cavity, between the lungs in the space known as the mediastinum. Figure 12.1 shows the position of the heart within the thoracic cavity. Within the mediastinum, the heart is separated from the other mediastinal structures by a tough membrane known as the pericardium, or pericardial sac, and sits in its own space called the pericardial cavity. The great vessels, which carry blood to and from the heart, are attached to the superior surface of the heart, which is called the base. The base of the heart is located at the level of the third costal cartilage. The inferior tip of the heart, the apex, lies just to the left of the sternum between the junction of the fourth and fifth ribs.
- On the diagram below (Figure 1), locate the mediastinum, the pericardial cavity, the base of the heart and the apex of the heart.
- Locate the largest vein in the body superior vena cava.
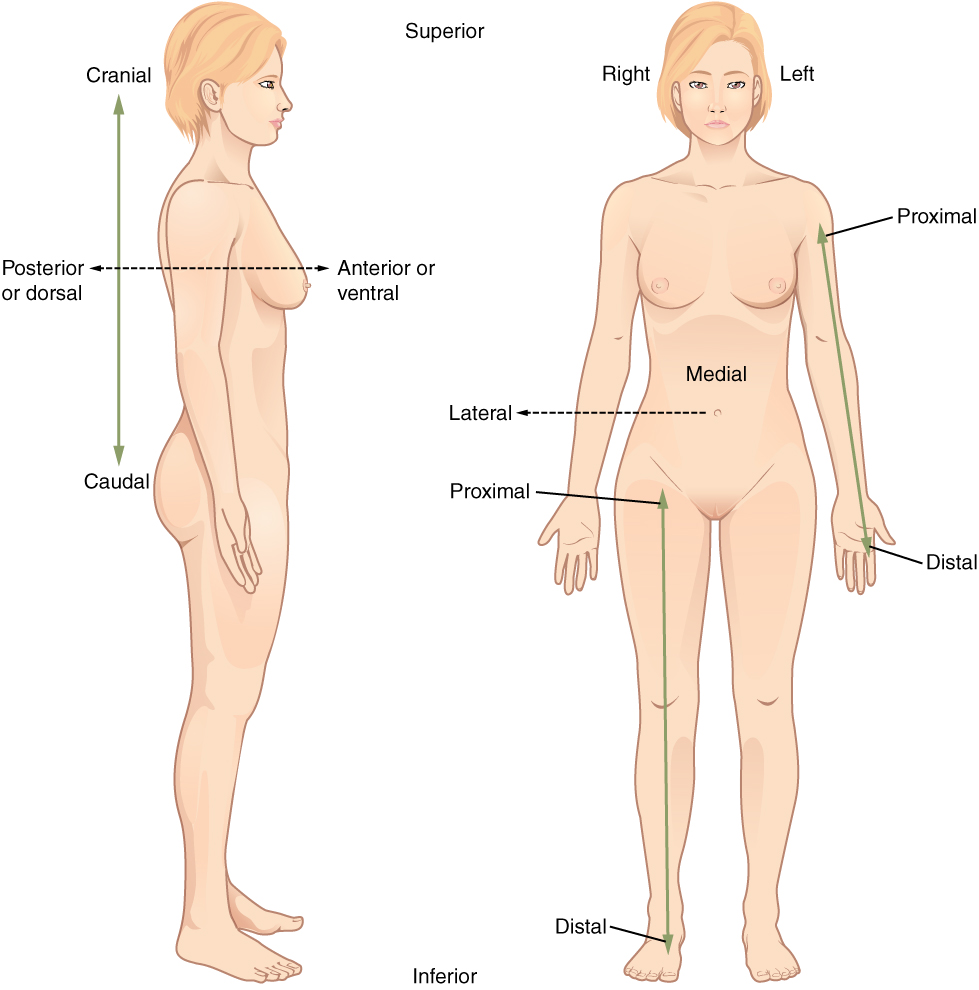
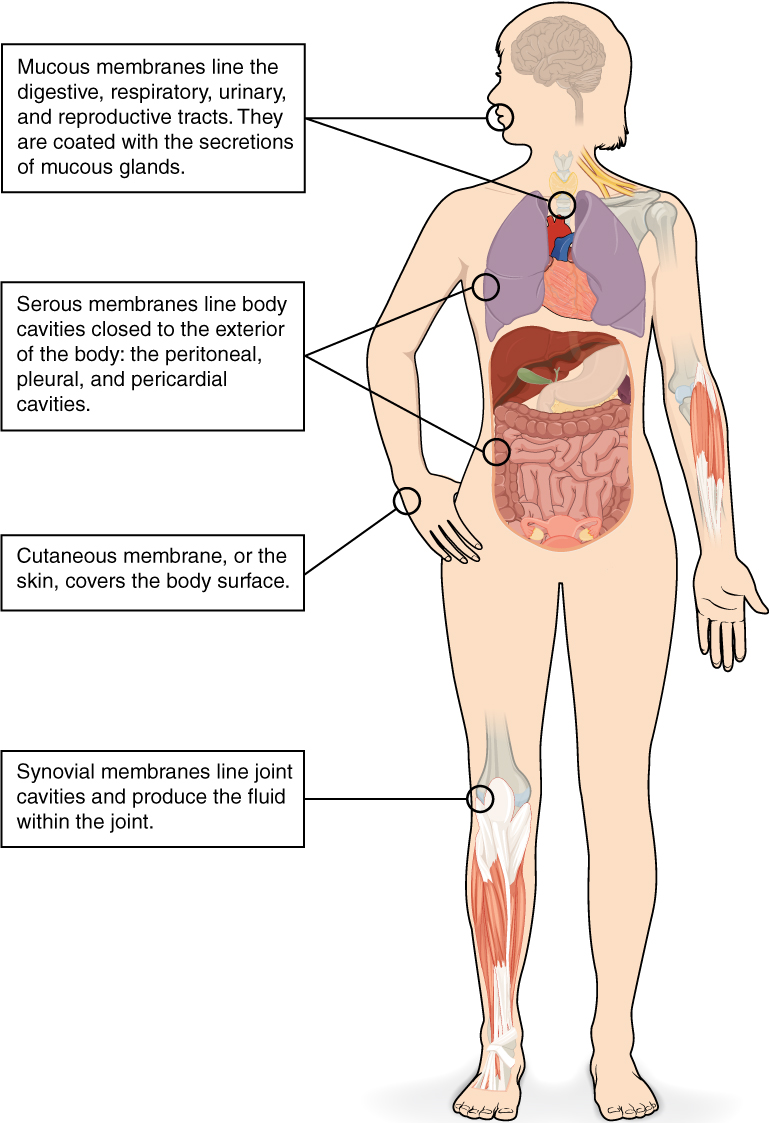
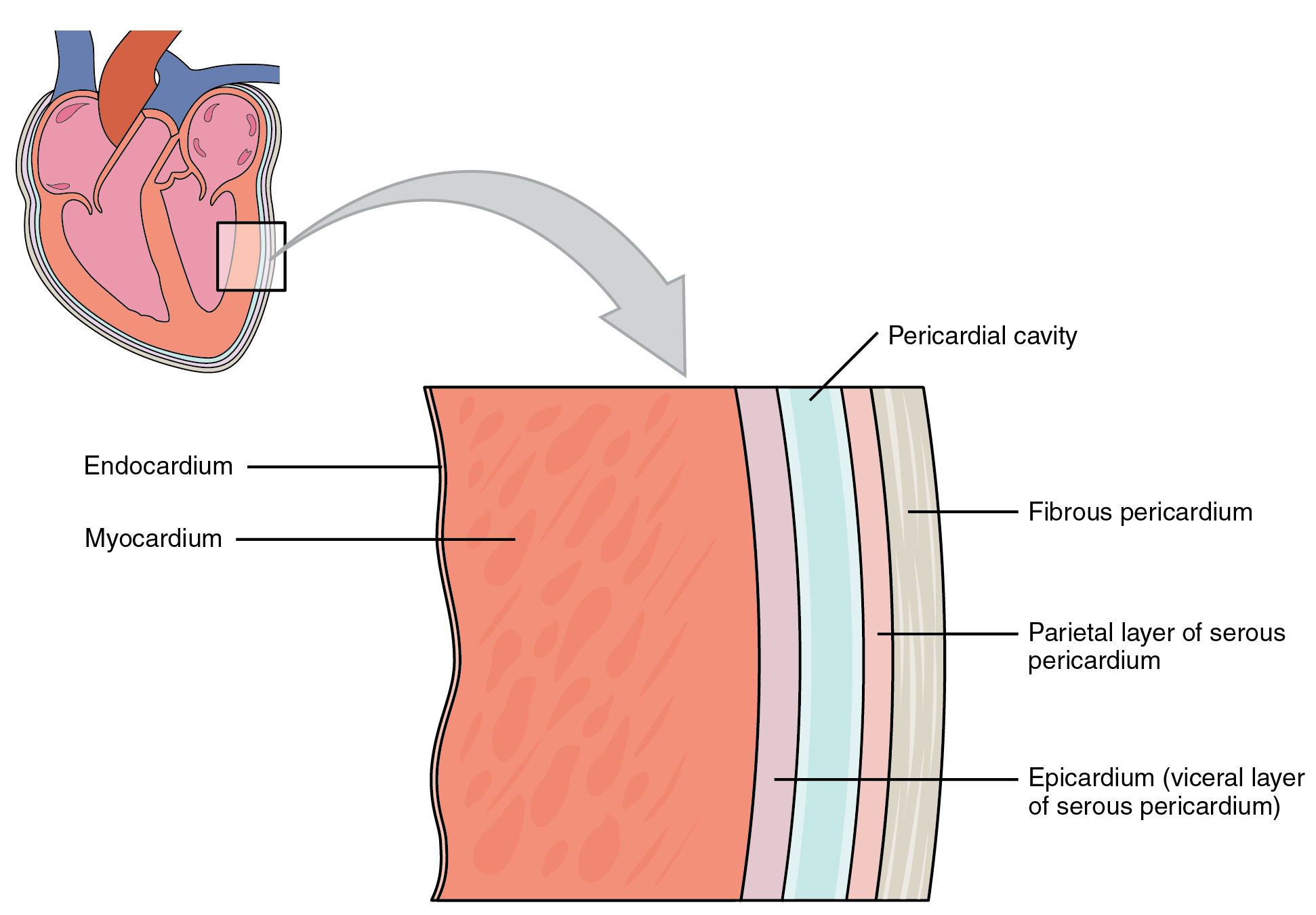
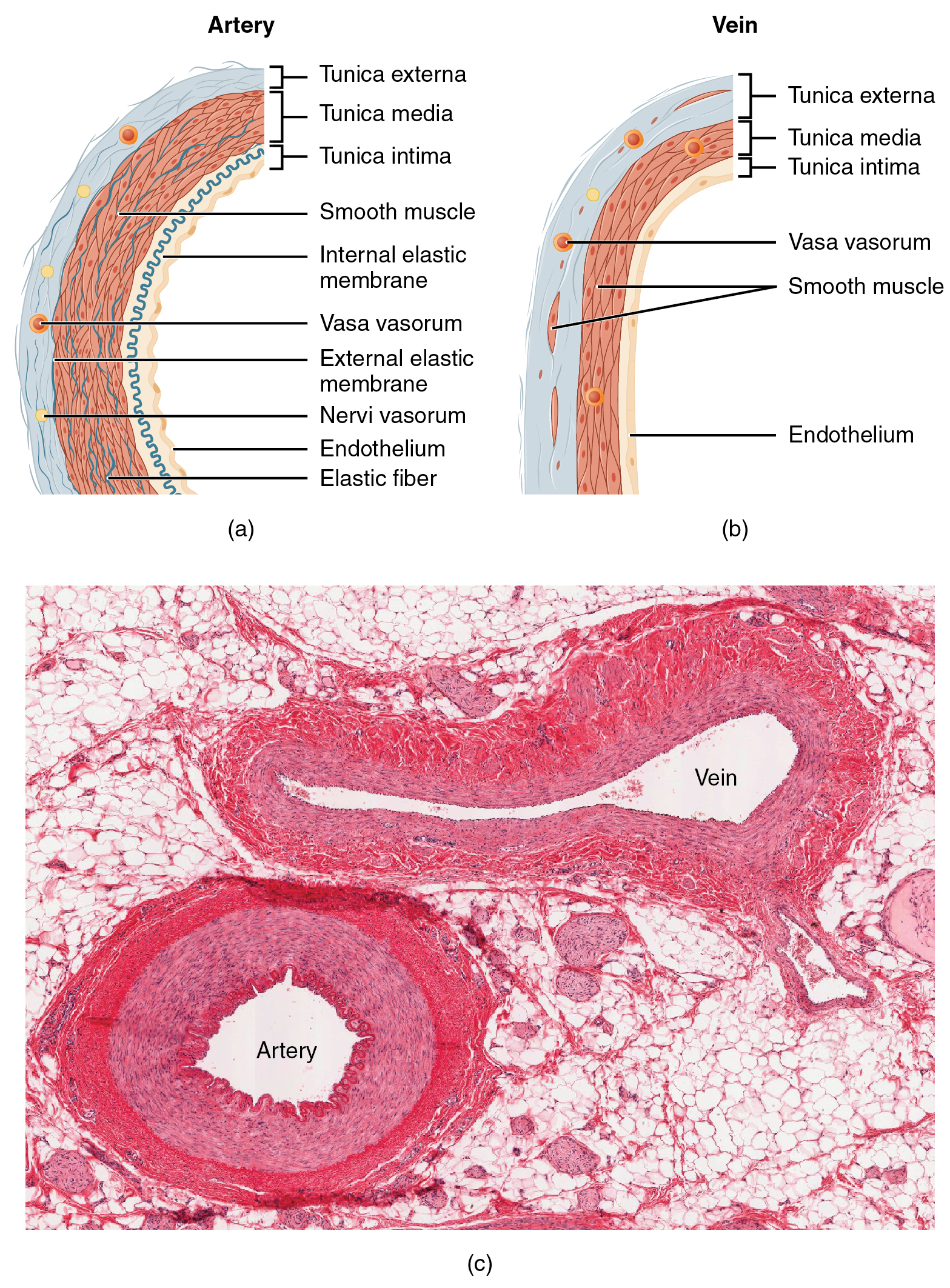
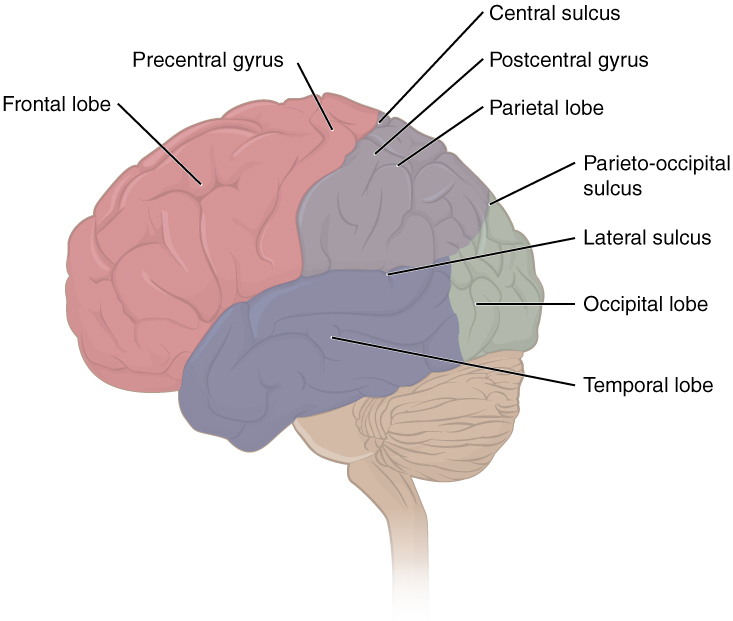
Membranes and Layers of the Heart Walls
The heart and the roots of the great vessels are surrounded by a membrane known as the pericardium or pericardial sac. The pericardium consists of two distinct sub layers:
- The sturdy outer fibrous pericardium is made of tough, dense connective tissue that protects the heart and holds it in position.
- Separated by the pericardial cavity and containing pericardial fluid the inner serous pericardium consists of two layers:
- the outer parietal pericardium, which is fused to the fibrous pericardium.
- the inner visceral pericardium, or epicardium, which is fused to the heart and forms the outer layer of the heart wall.
The walls of the heart consist of three layers:
- The outer epicardium, which is another name for the visceral pericardium mentioned above.
- The thick, middle myocardium, which is made of muscle tissue and gives the heart its ability to contract.
- The inner endocardium, which lines the heart chambers and is the main component of the heart valves.
- Look at Figure 12.2 below, and name the layers of the heart wall and surrounding membranes, starting with the innermost layer.
- As shown on the diagram, suggest why is the myocardium layer is thicker than the endocardium layer?
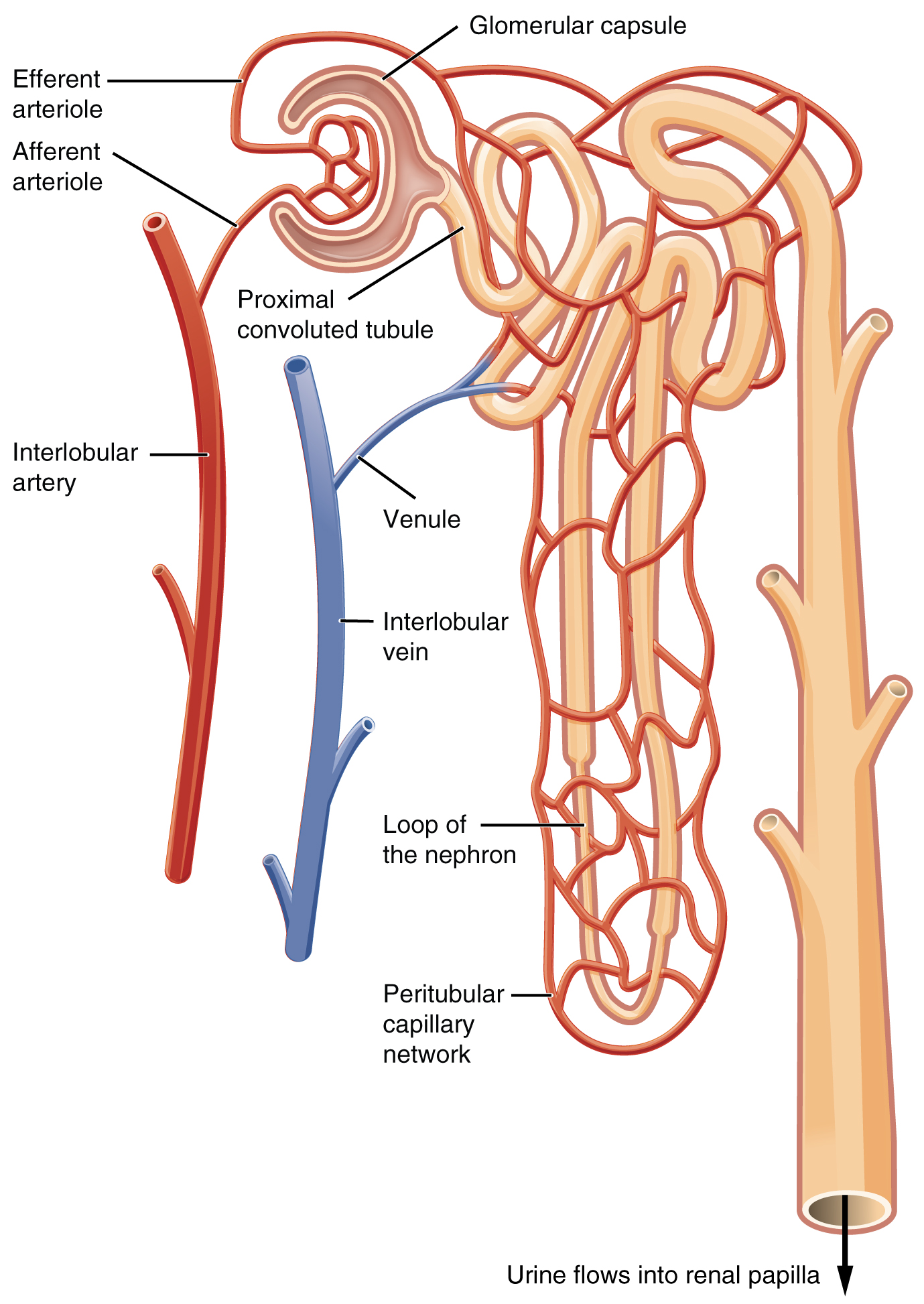
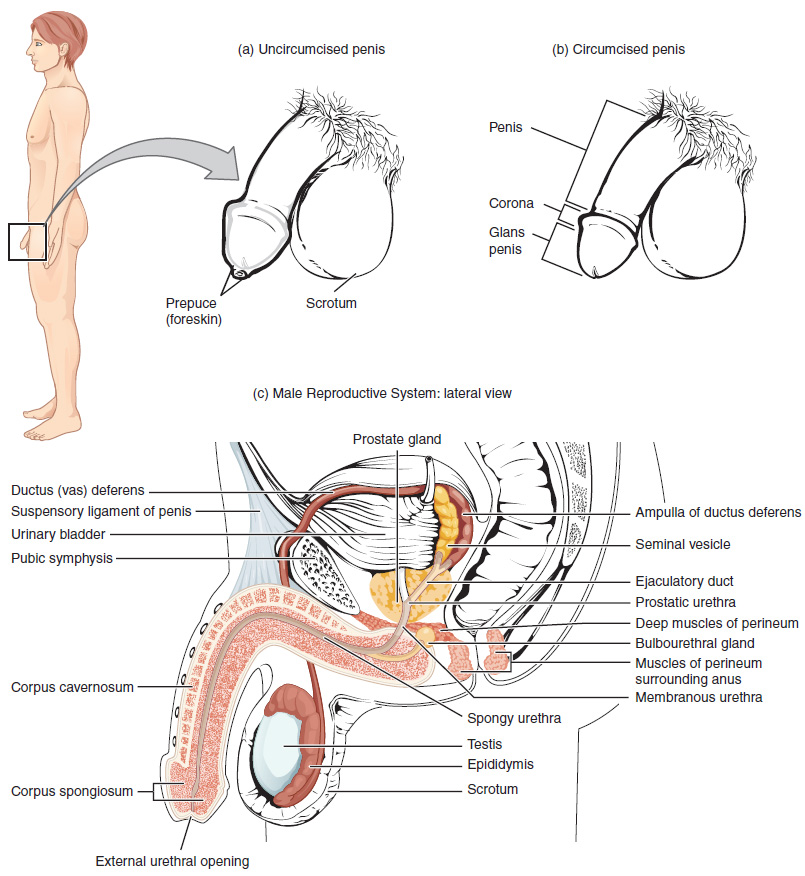
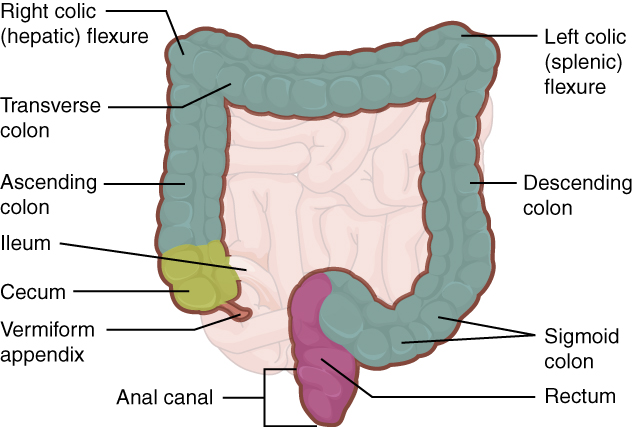
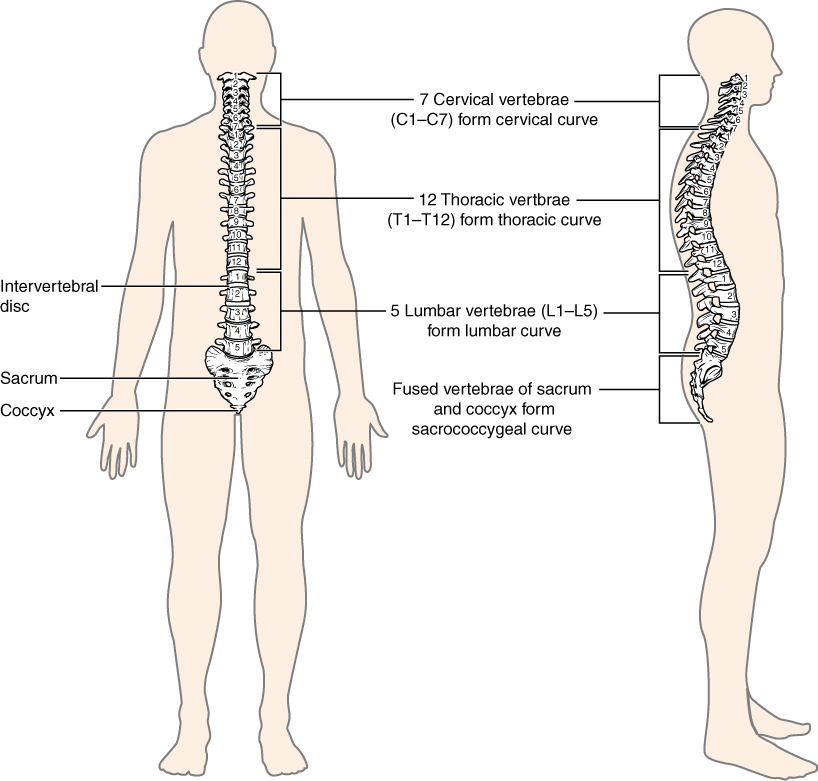
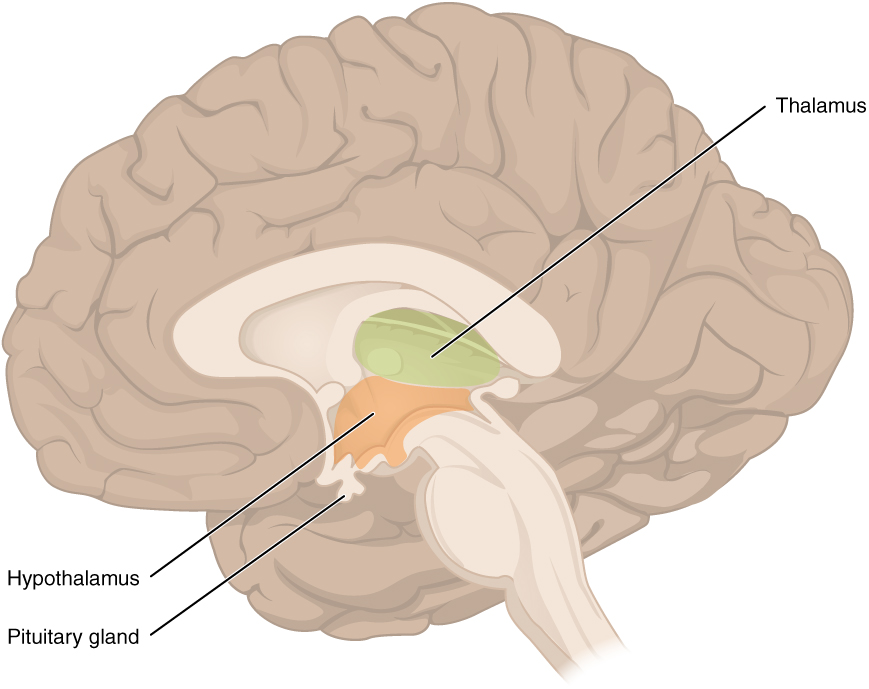
Internal Structures of the Heart
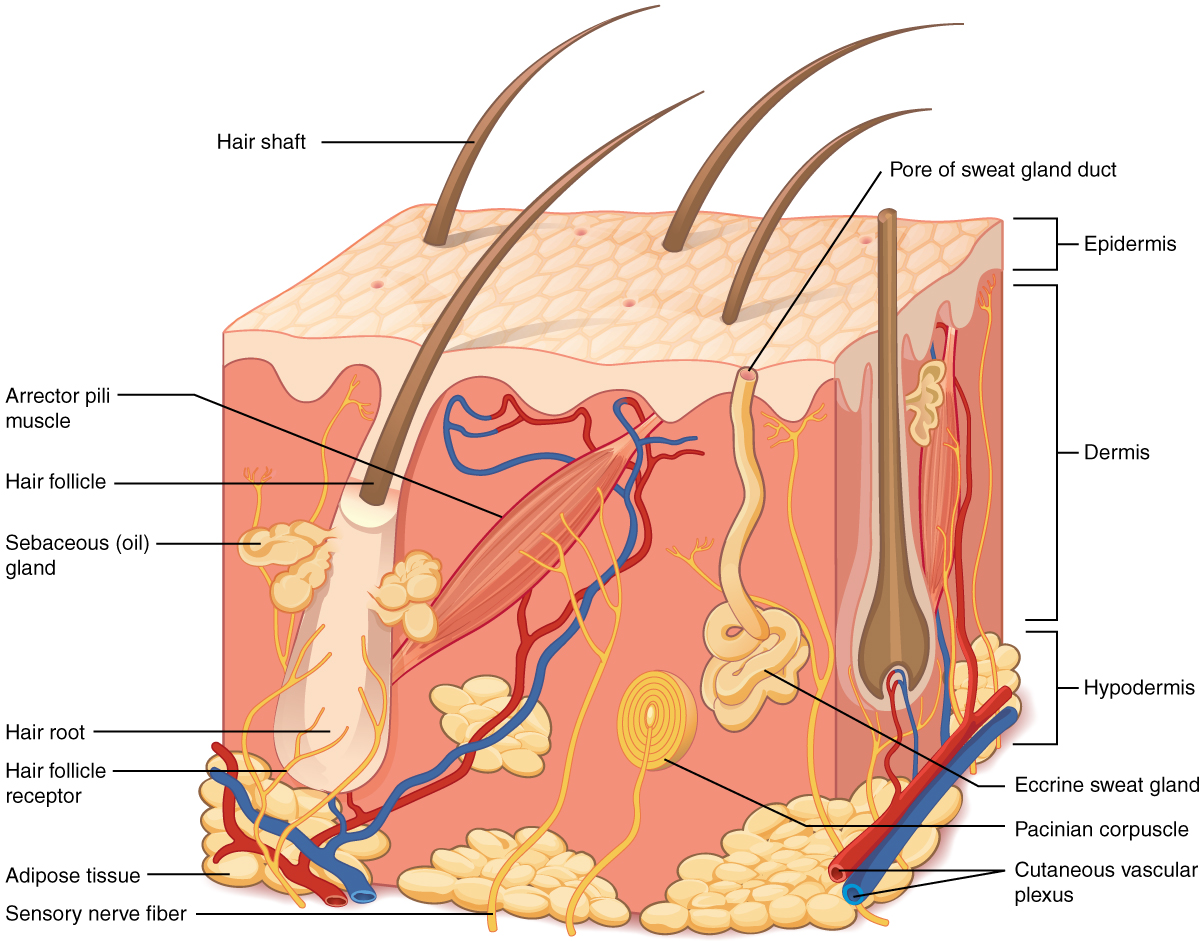
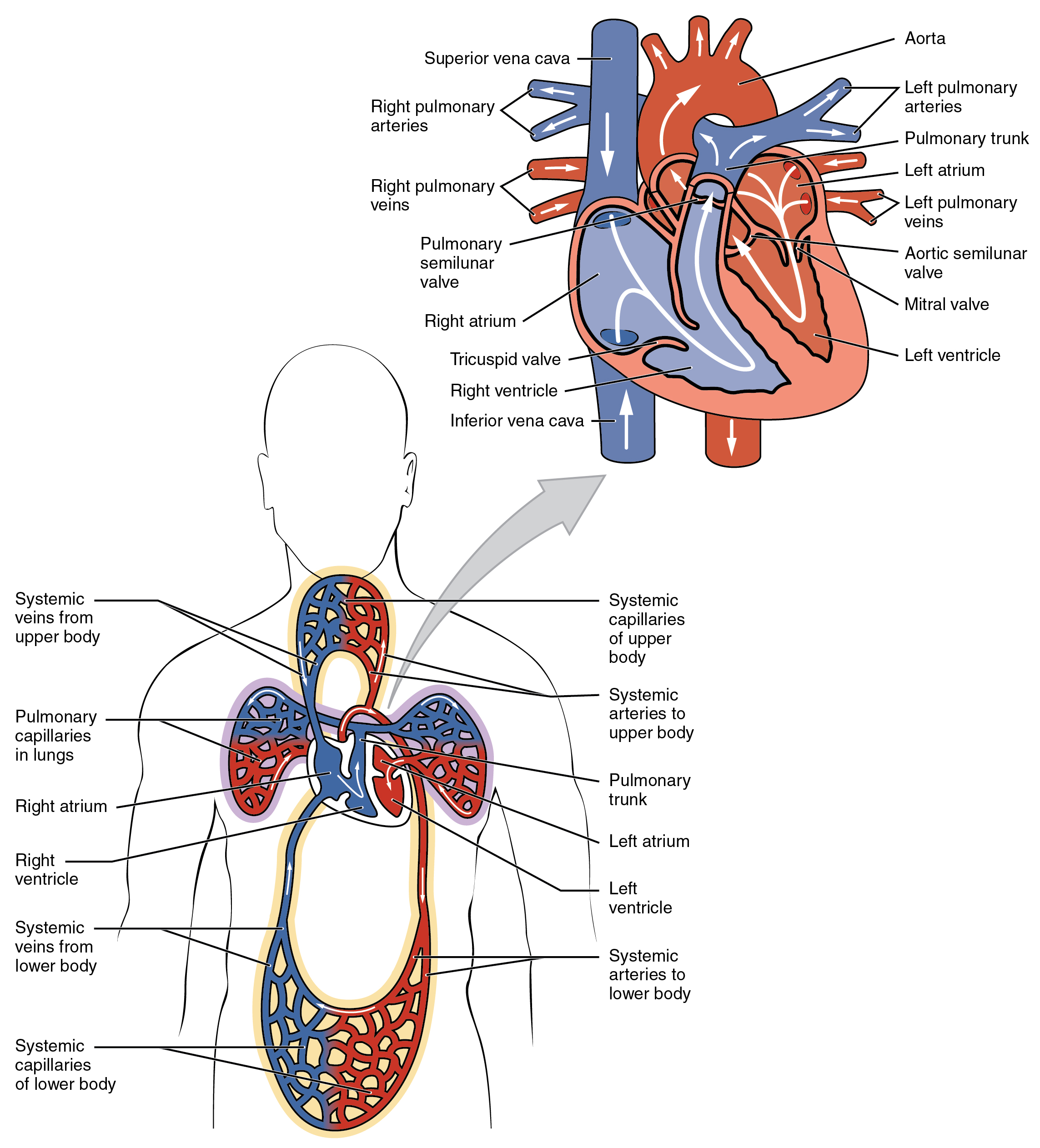
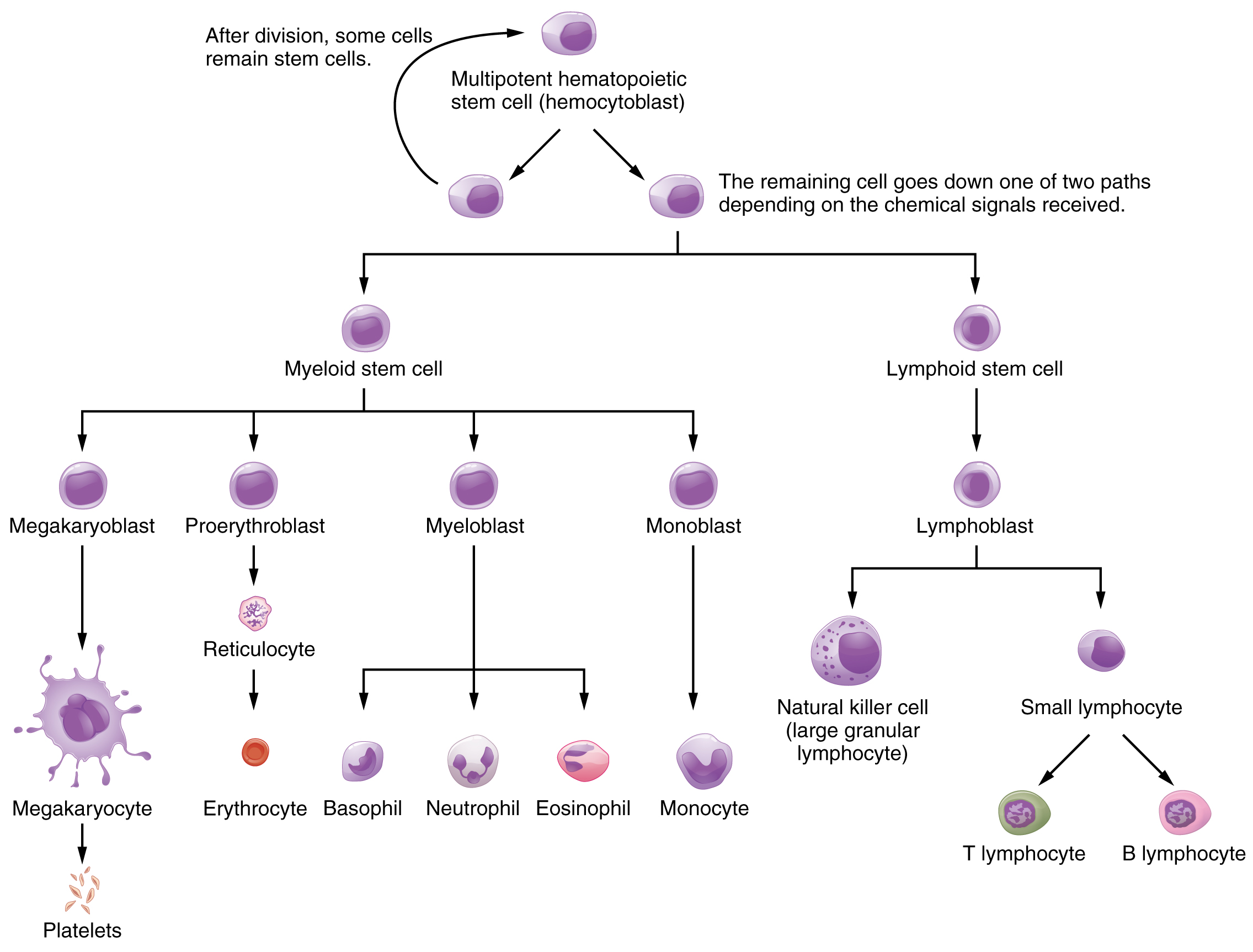
The heart consists of four chambers:
- The upper chambers are the right and left atria (singular: atrium).
- The lower chambers are the right and left ventricles.
The interventricular septum is a muscular wall that separates the right and left ventricles. The interatrial septum separates the right and left atria.
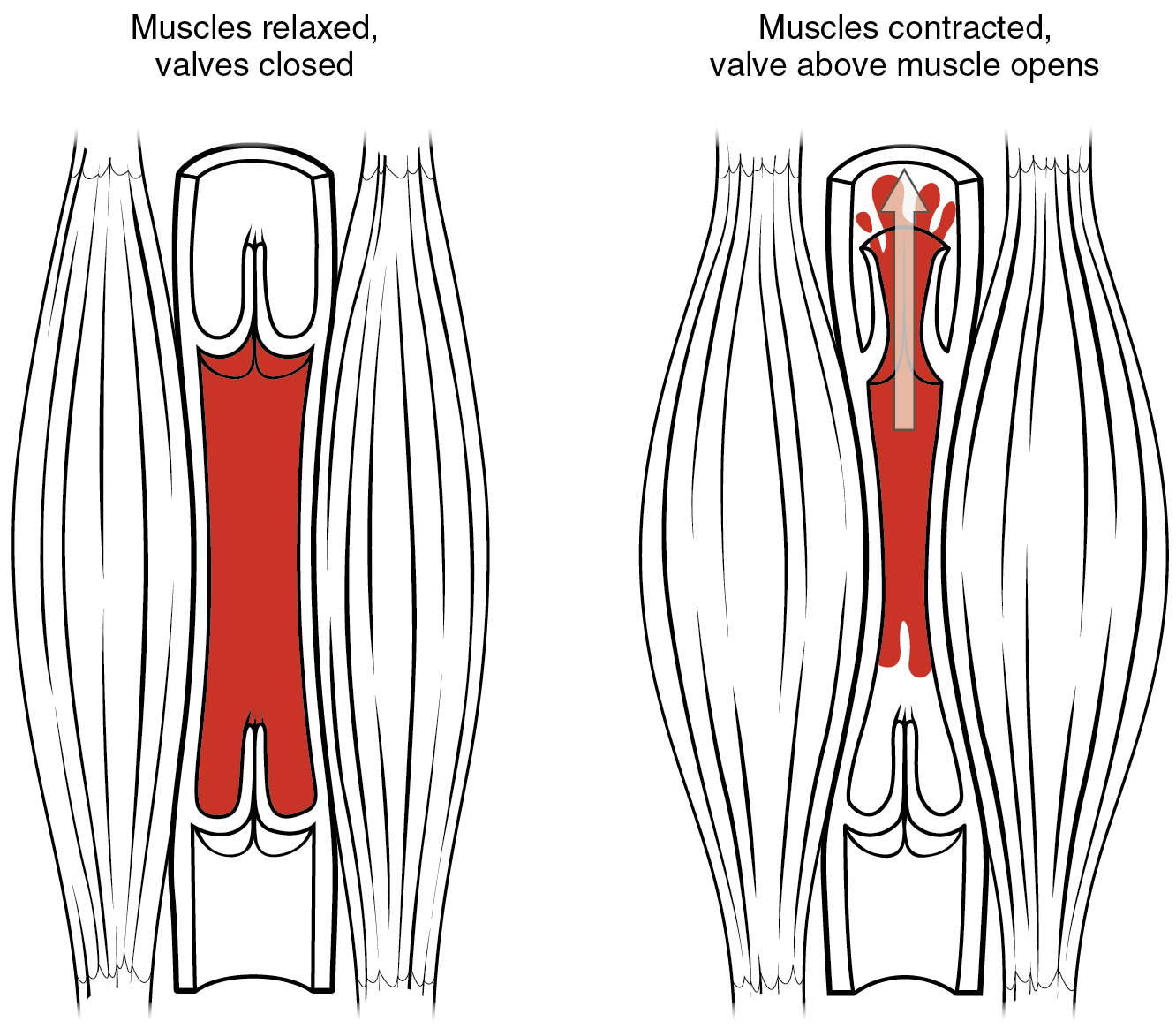
The atrium and ventricle on each side of the heart are separated by an atrioventricular (AV) valve:
- The right AV valve, or tricuspid valve, separates the right atrium and right ventricle.
- The left AV valve, or bicuspid valve, separates the left ventricle and the left atrium. This valve is also called the mitral valve.
There are also two semilunar valves:
- The pulmonary valve separates the right ventricle from the pulmonary trunk.
- The aortic valve separates the left ventricle from the aorta (De Saix, et al., 2013).
Anatomy Labeling Activity
An interactive or media element has been excluded from this version of the text. You can view it online here:
https://ecampusontario.pressbooks.pub/medicalterminology/?p=259
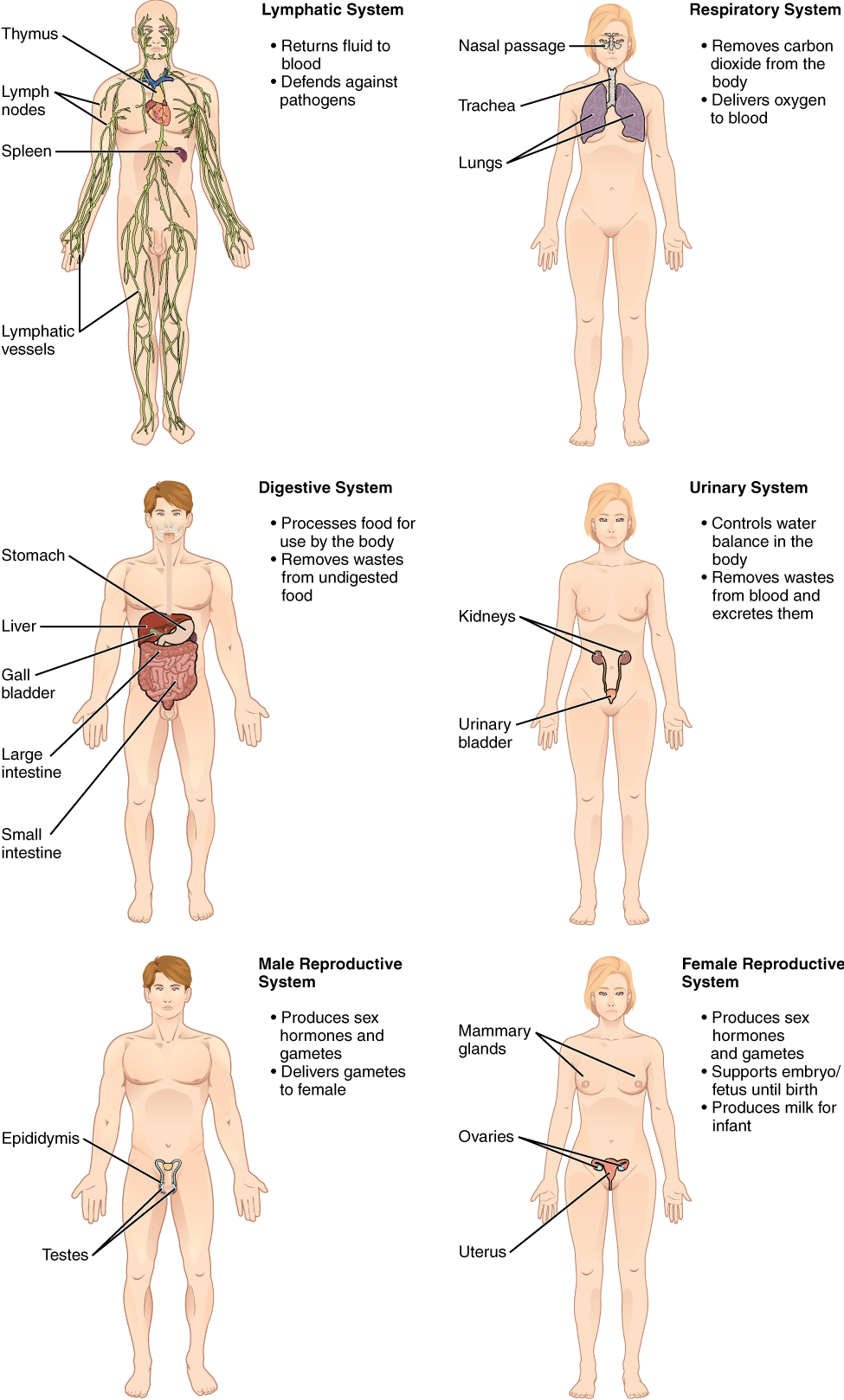
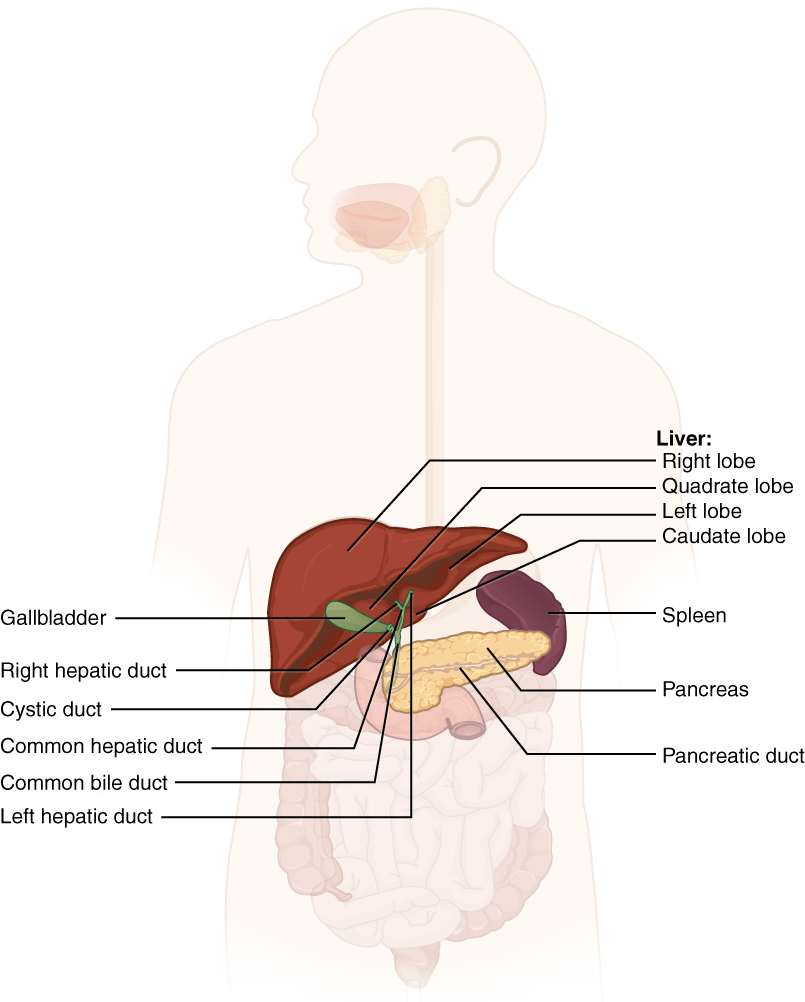
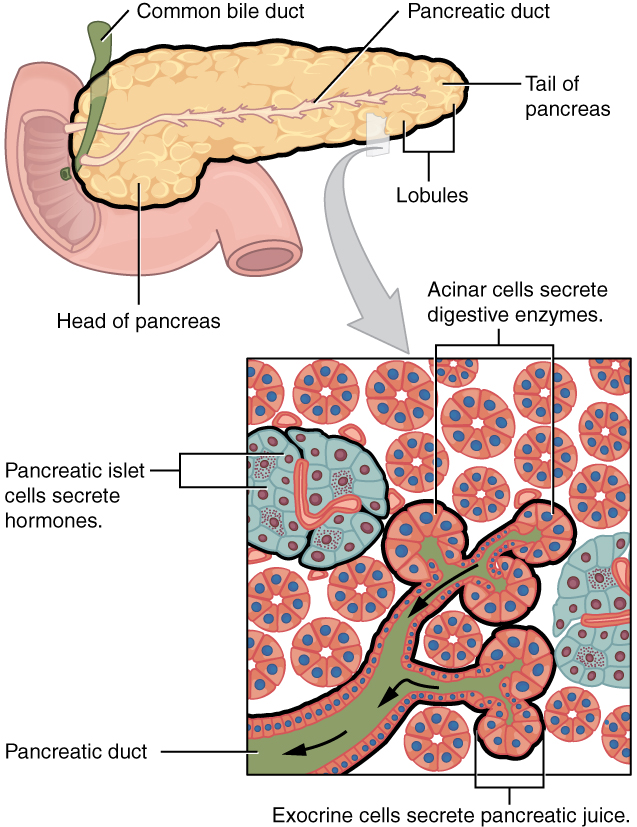
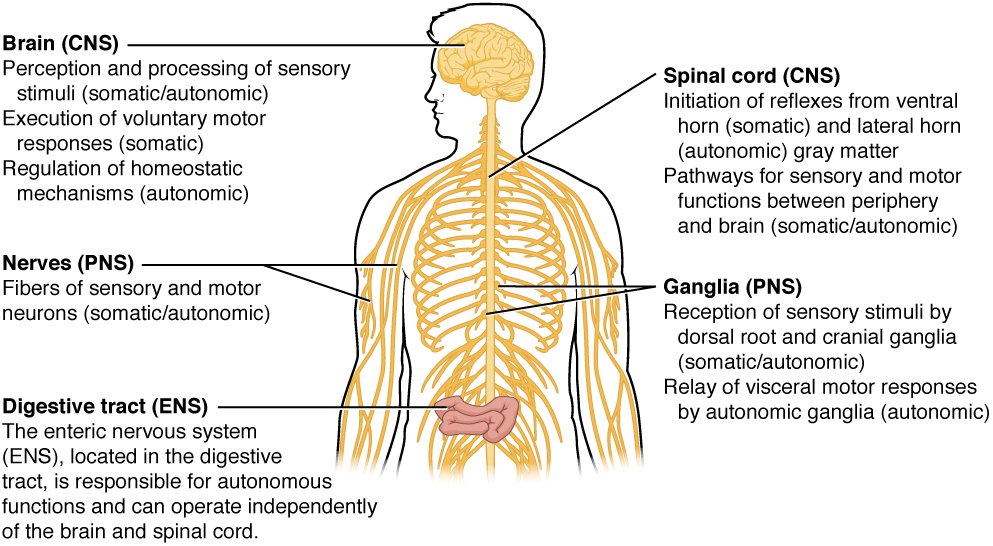
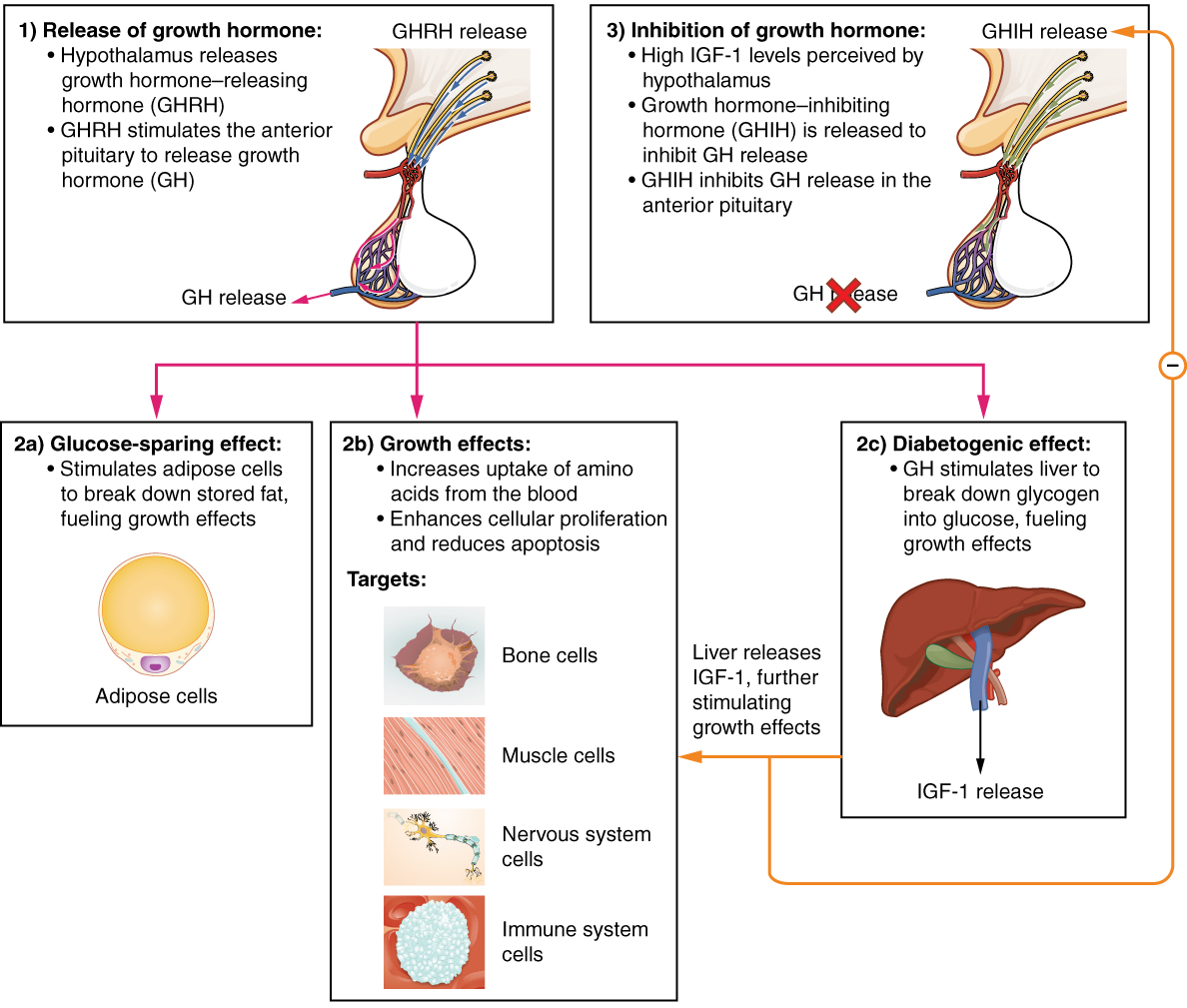
Physiology of the Heart
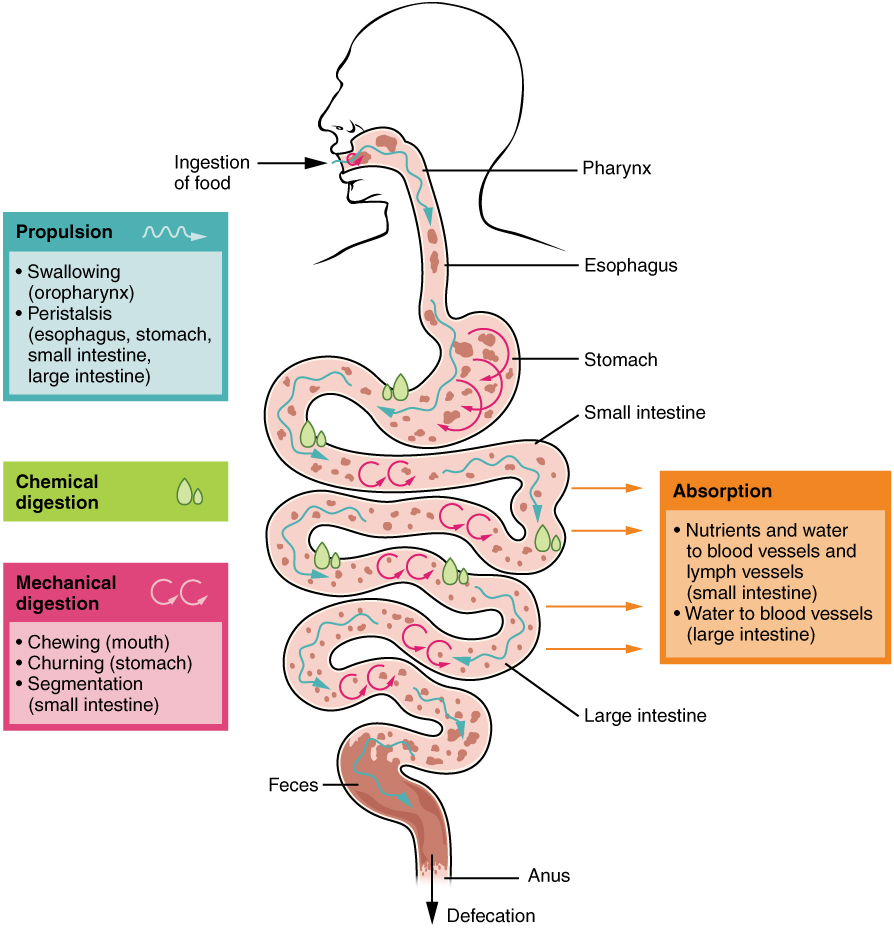
In order for the heart to do its job of pumping blood to the lungs and to the body, nutrients and oxygen must be supplied to the cells of the heart. The heart also needs to coordinate its contractions so that all parts are working together to pump blood effectively. To understand how all of this works together to give the heart its ability to pump blood, we will examine three interdependent aspects of heart function.
- Circulation through the heart: Blood is pumped by the heart in order to provide oxygen and nutrients to every cell in the body.
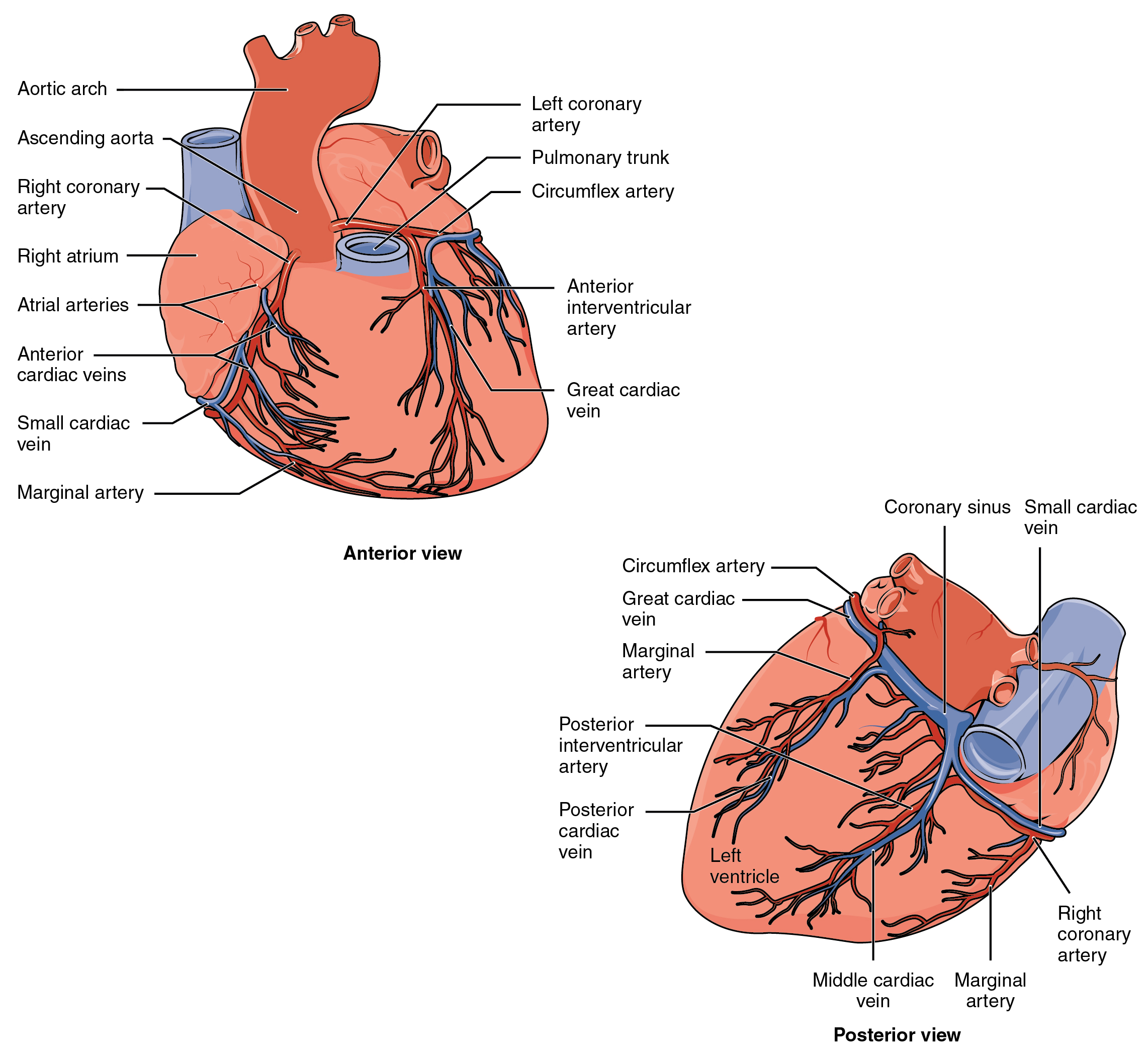
- The heart as an organ (coronary blood supply): The heart is an organ, made of cells and tissues which require their own blood supply.
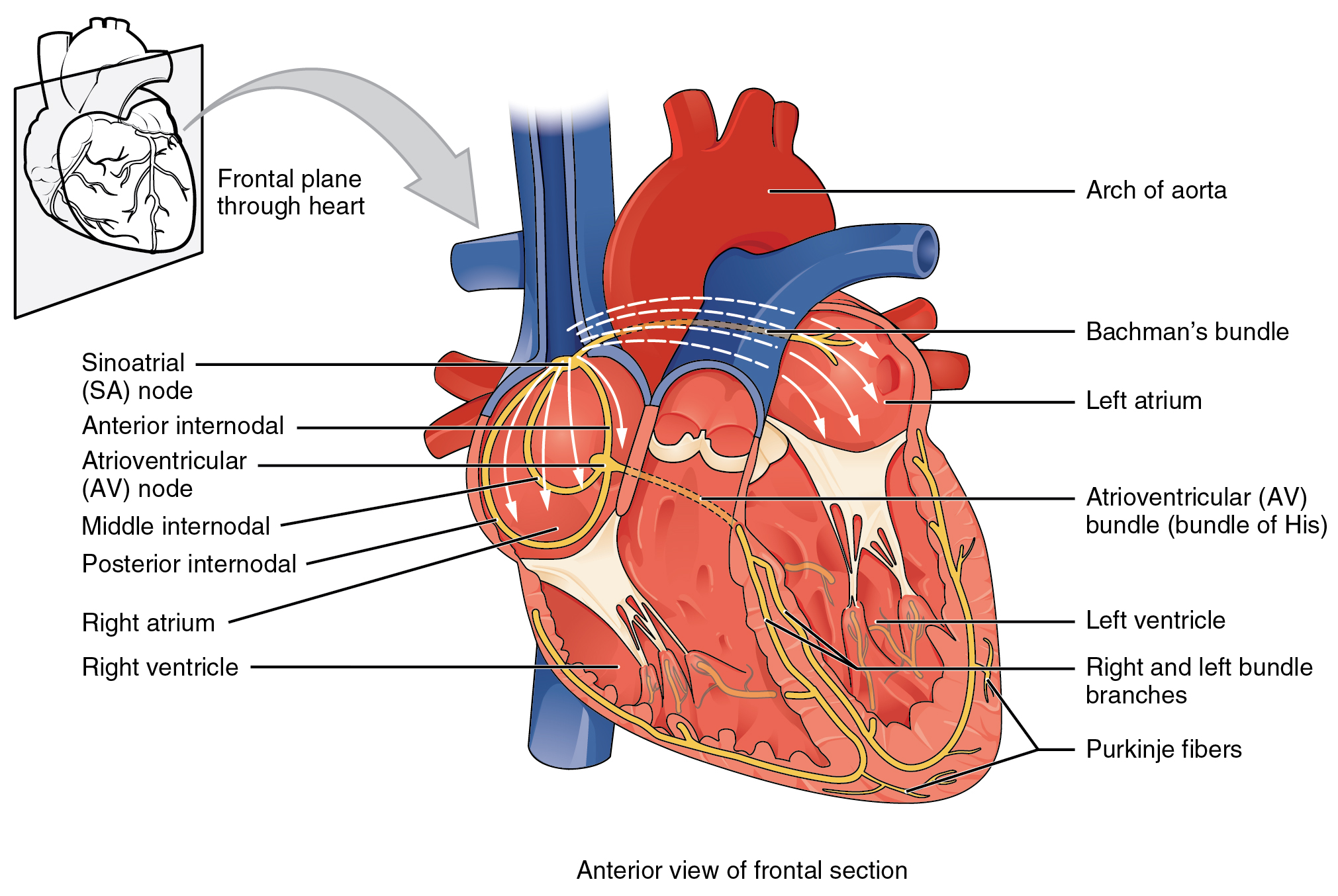
- The heart’s electrical conduction system: The heart is able to independently generate and transmit instructions to the myocardium, in order to make it contract and pump the blood.
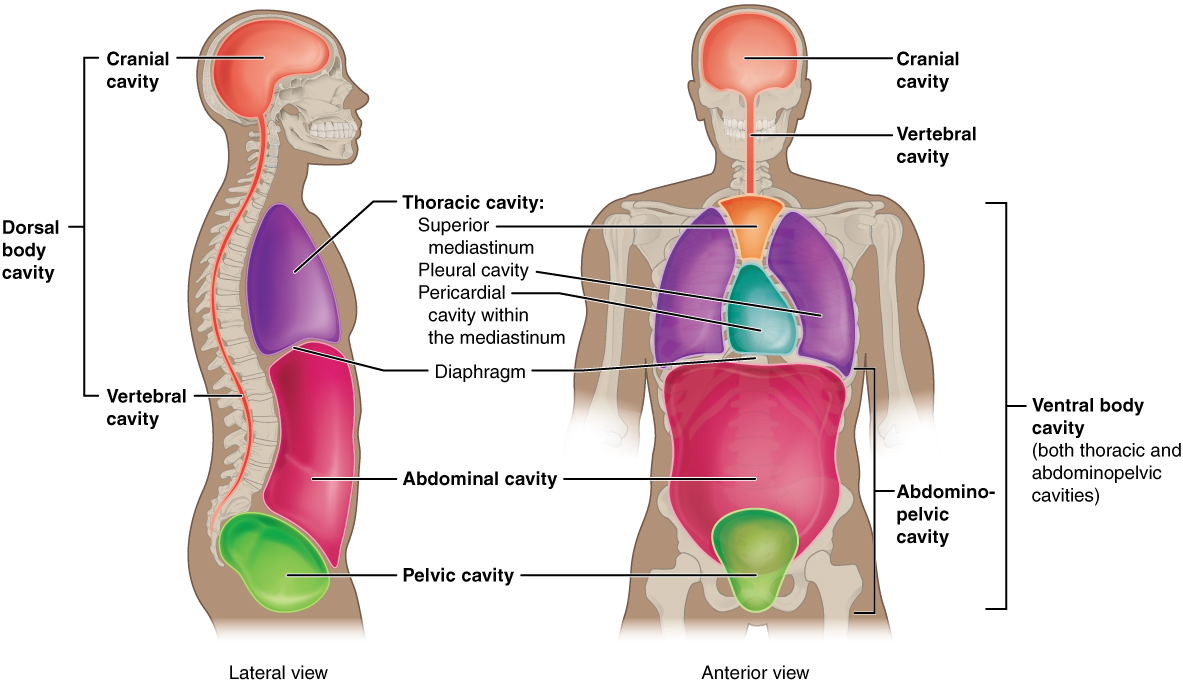
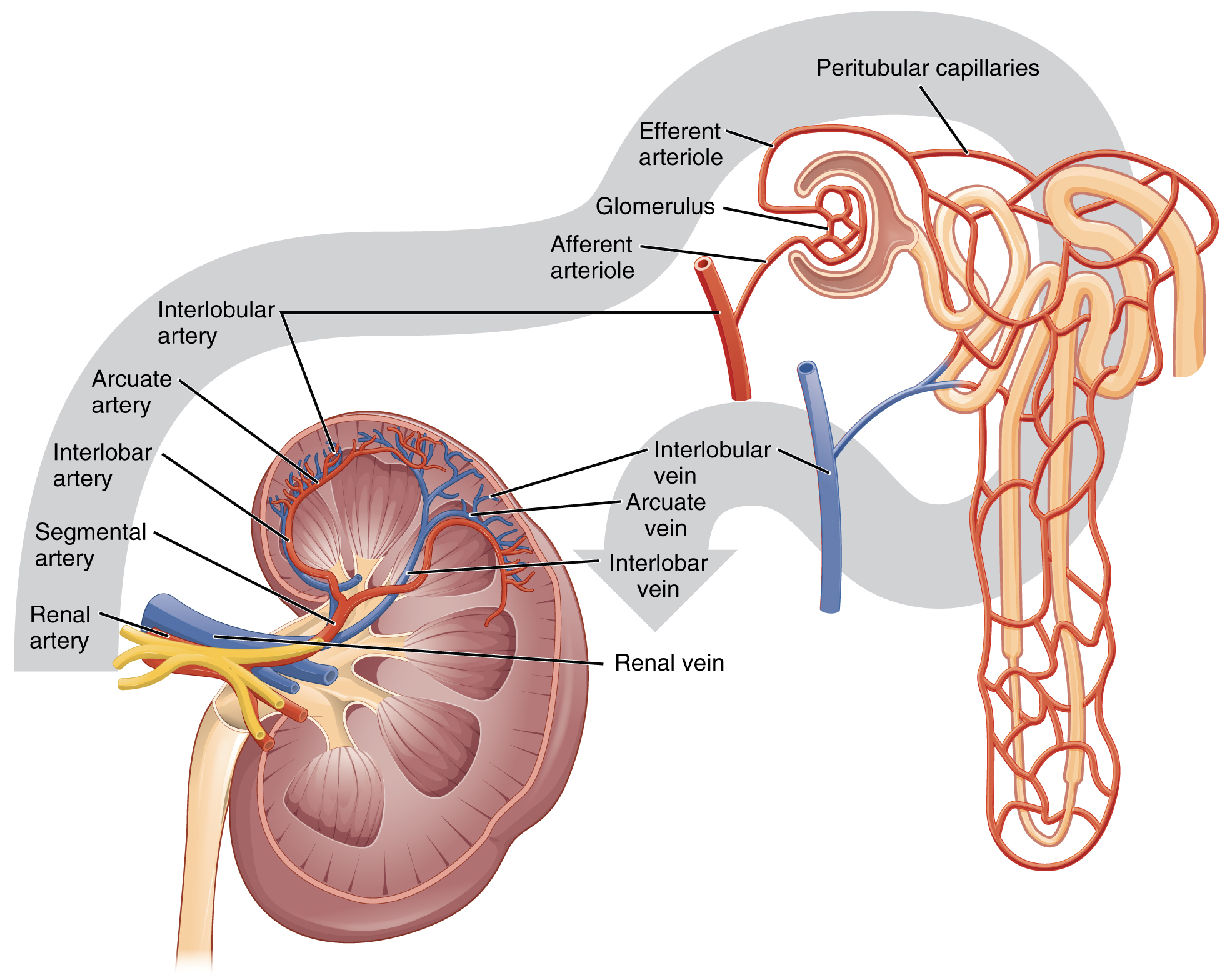
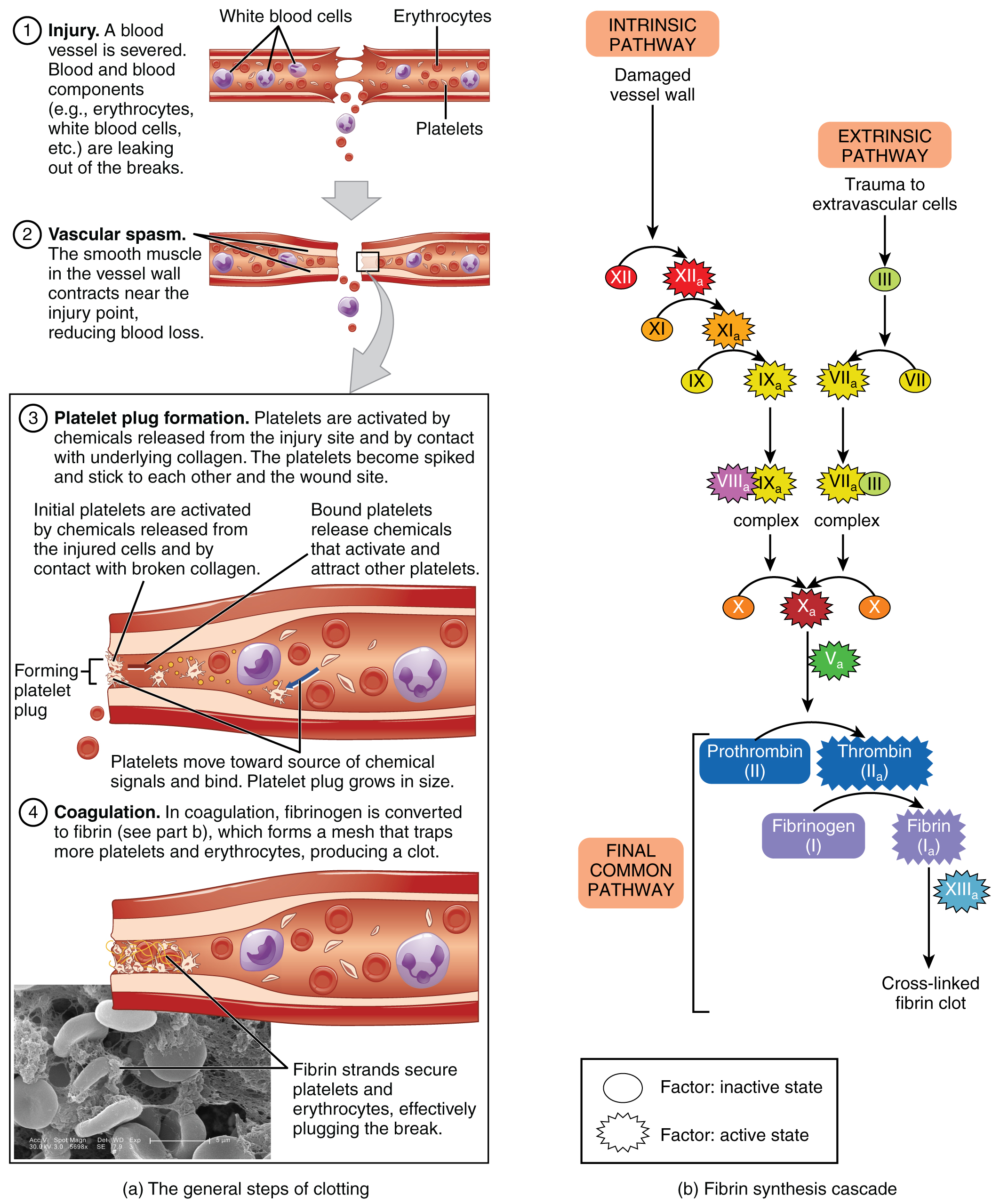
1. Circulation Through the Heart: The Heart as a Pump
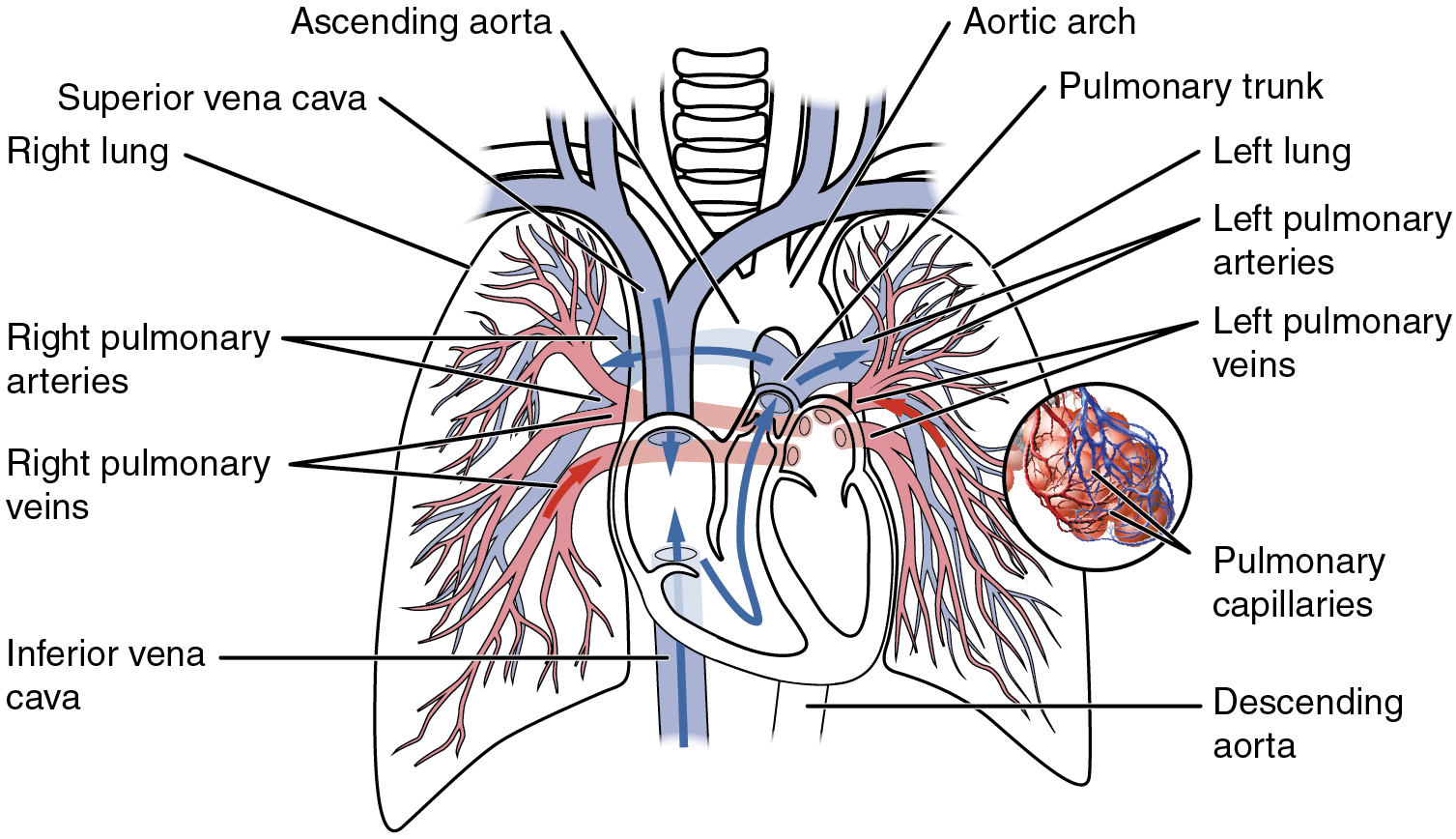
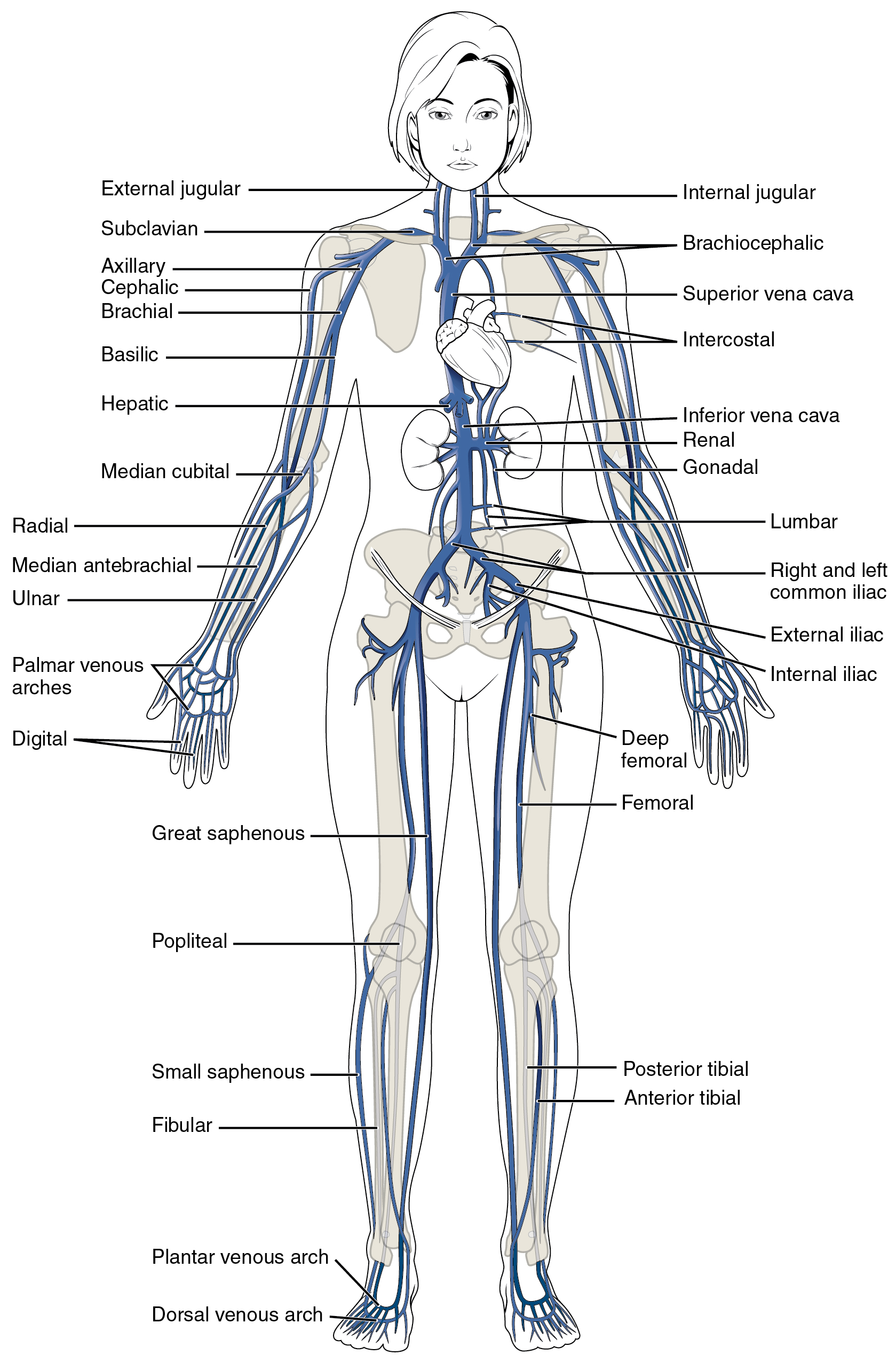
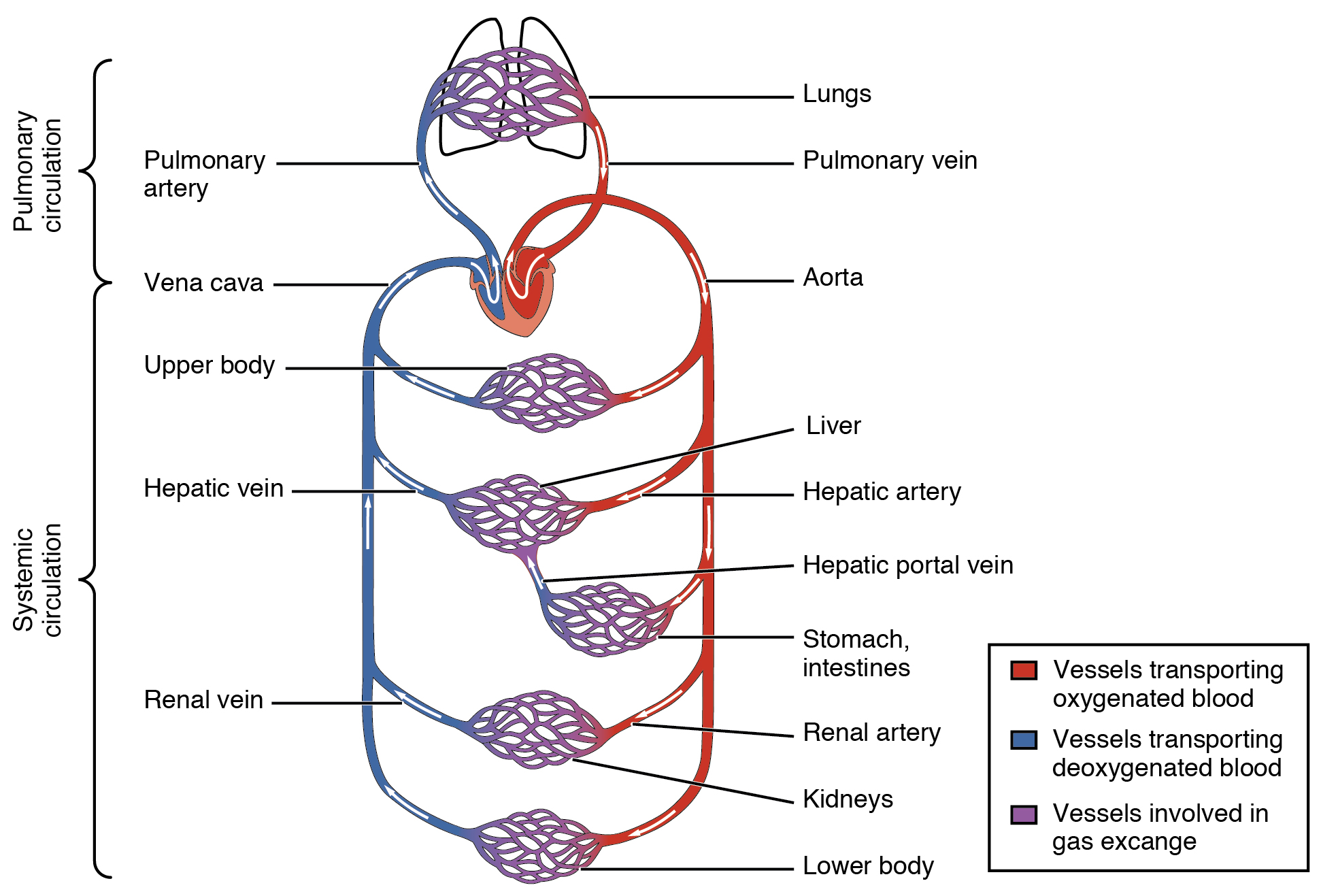
The heart pumps blood to two distinct but linked circulatory systems called the pulmonary and systemic circuits. The pulmonary circuit transports blood to and from the lungs, where it picks up oxygen and drops off carbon dioxide. The systemic circuit transports freshly oxygenated blood to virtually all of the tissues of the body and returns relatively deoxygenated blood and carbon dioxide to the heart to be sent back to the pulmonary circulation.
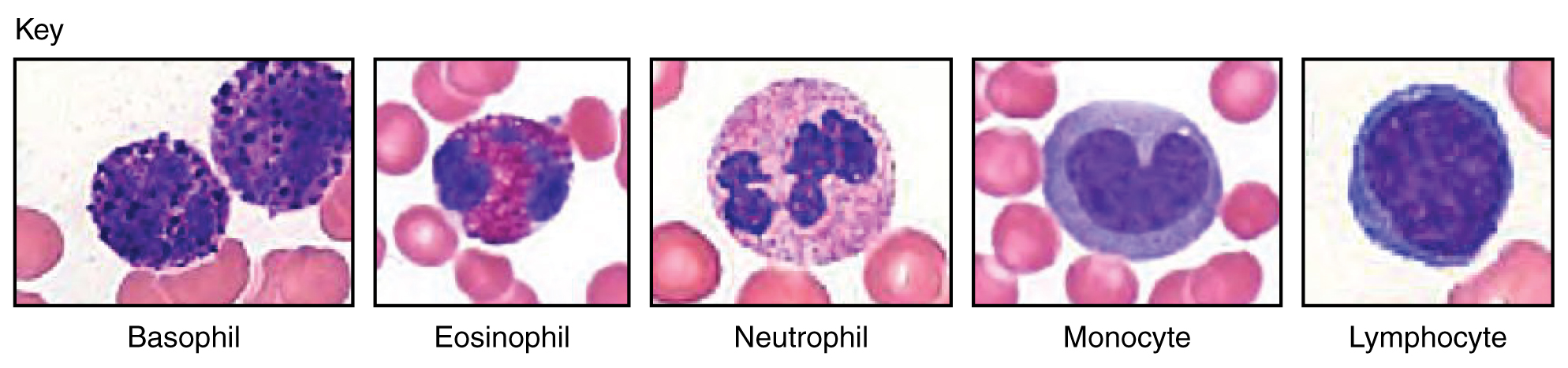
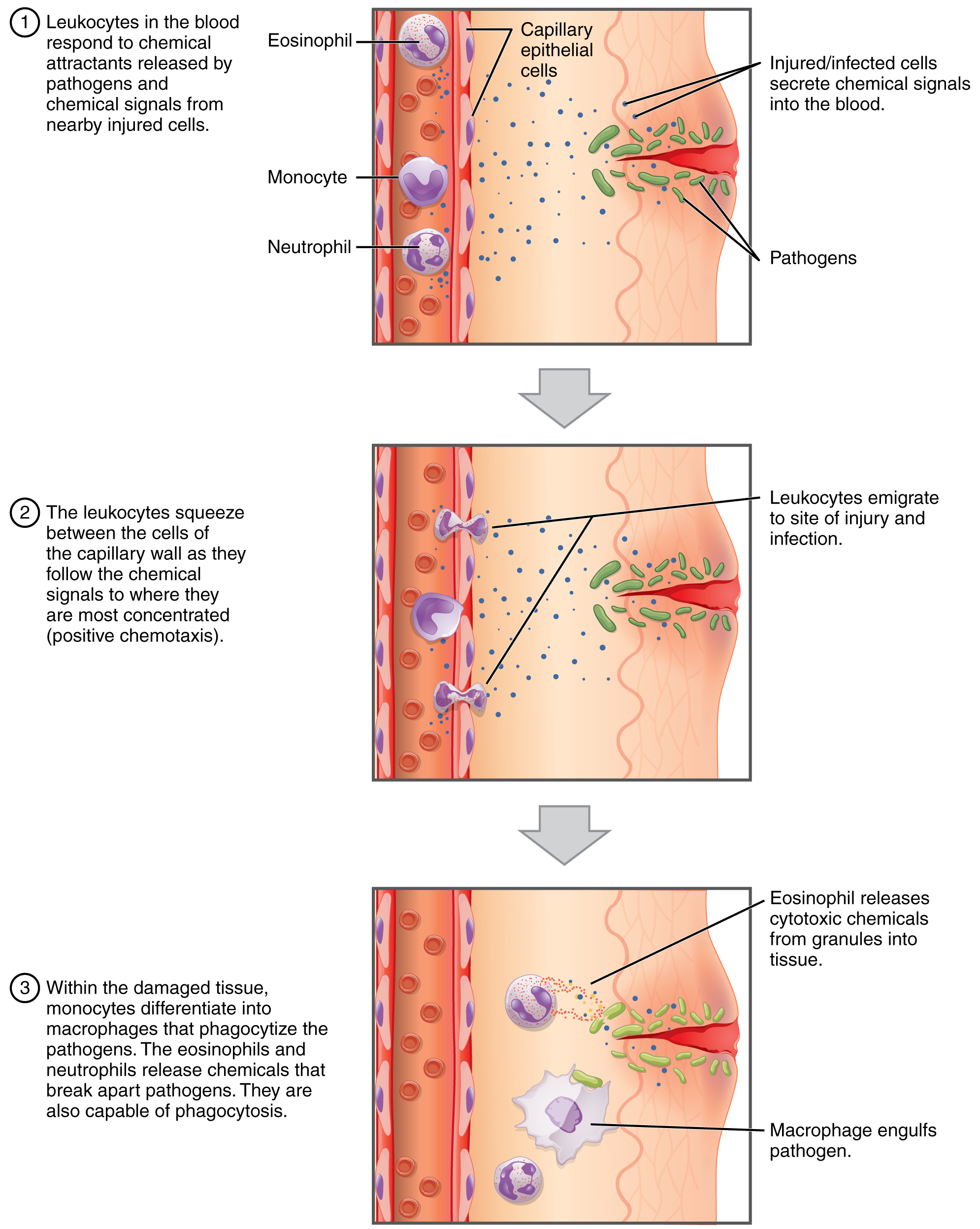
- Blood that is carrying carbon dioxide and waste products from the body tissues is returned to the right atrium via the superior vena cava and the inferior vena cava.
- From the right atrium, the deoxygenated blood moves through the tricuspid valve into the right ventricle.
- The right ventricle pumps deoxygenated blood through the pulmonary valve into the pulmonary trunk, which splits into the right and left pulmonary arteries, leading toward the lungs. These arteries branch many times before reaching the pulmonary capillaries, where gas exchange occurs: carbon dioxide exits the blood and oxygen enters. The pulmonary arteries are the only arteries in the postnatal body that carry deoxygenated blood. Did you notice that they are often coloured blue on diagrams of the heart?
- Freshly oxygenated blood returns from the lungs to the left atrium via the pulmonary veins. These veins only postnatal veins in the body that carry highly oxygenated blood, and are often coloured red on heart images.
- From the left atrium, the blood moves through the mitral valve into the left ventricle.
- The left ventricle pumps blood through the aortic valve, into the aorta, delivering blood to all parts of the body.
- On Figure 12.3 below, use your finger to trace the pathway of blood flowing through the right side of the heart, naming each each of the following structures as you encounter them: Superior and inferior venae cavae, right atrium, tricuspid valve, right ventricle, pulmonary valve, right and left pulmonary arteries.
- Suggest what would happen if the aorta experienced a blockage or constriction.
Watch this video:

A YouTube element has been excluded from this version of the text. You can view it online here: https://ecampusontario.pressbooks.pub/medicalterminology/?p=259
Media 12.2. The Heart, Part 2 – Heart Throbs: Crash Course A&P #26 [Online video]. Copyright 2015 by CrashCourse.
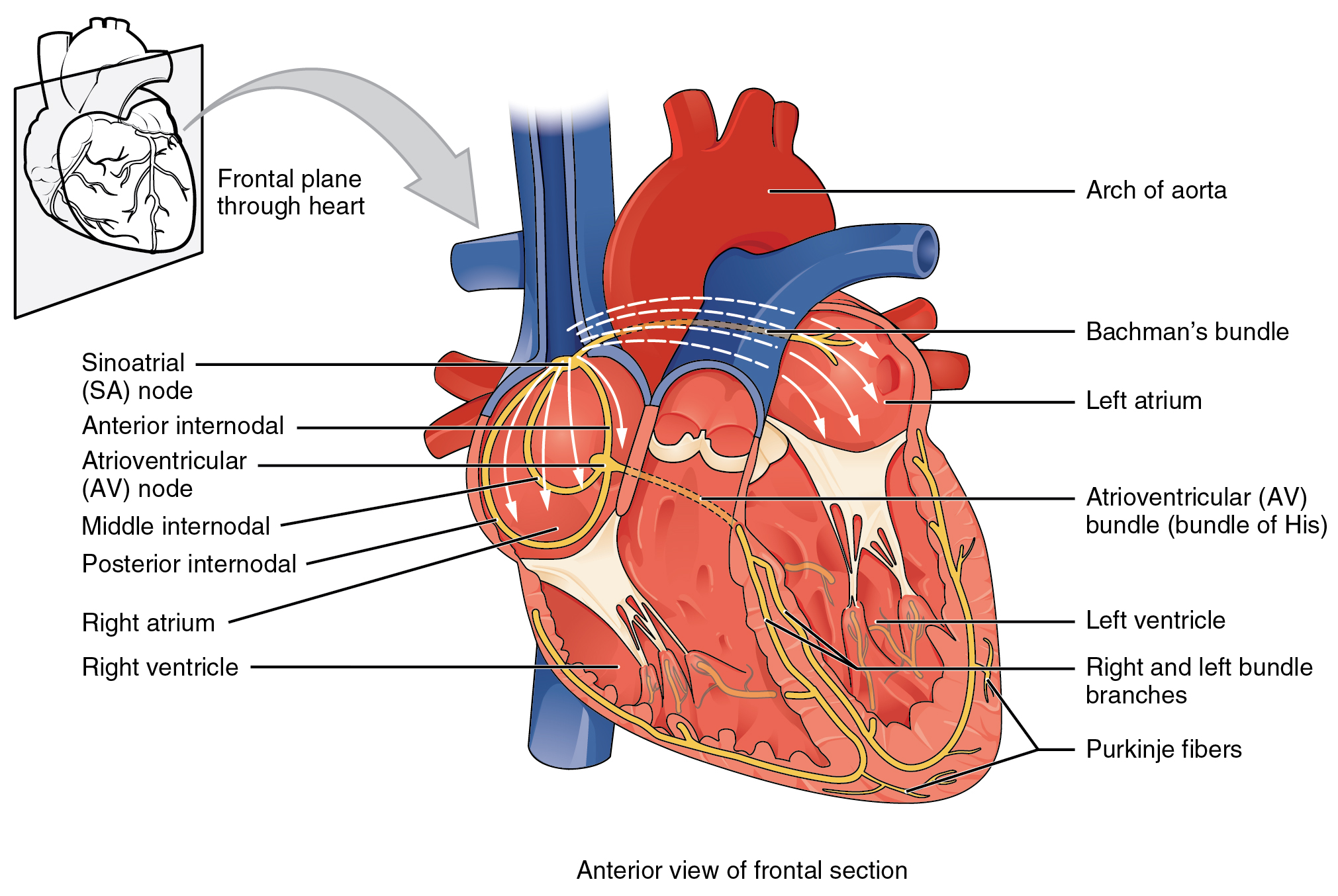
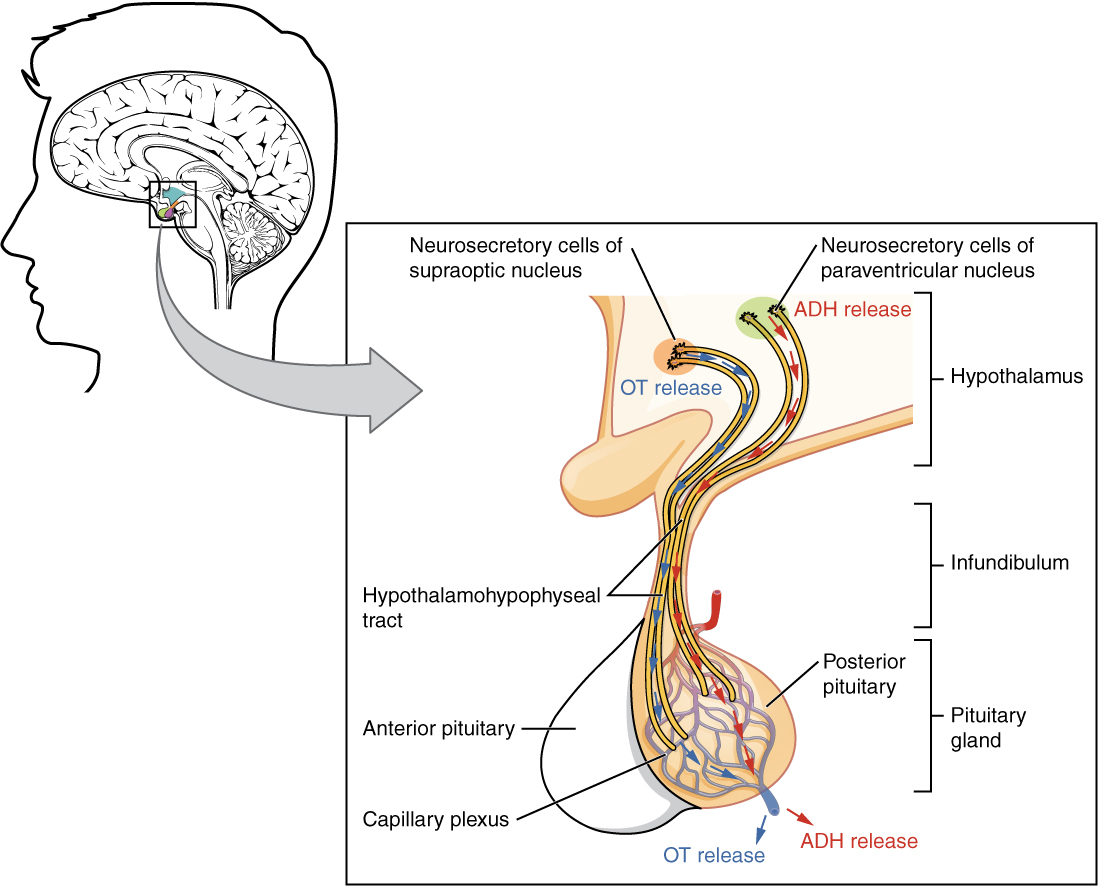
Figure 12.6. Conduction System of the Heart. Specialized conducting components of the heart include the sinoatrial node, the internodal pathways, the atrioventricular node, the atrioventricular bundle, the right and left bundle branches, and the Purkinje fibers. From Betts, et al., 2013. Licensed under
CC BY 4.0.
[Image description.] - On the image above, trace the electrical impulse generated by the heart’s pacemaker (the sinoatrial node, or SA node) through the rest of the conduction system, including the atrioventricular (AV) node, the atrioventricular bundle (bundle of His), the right and left bundle branches, and the Purkinje fibers.
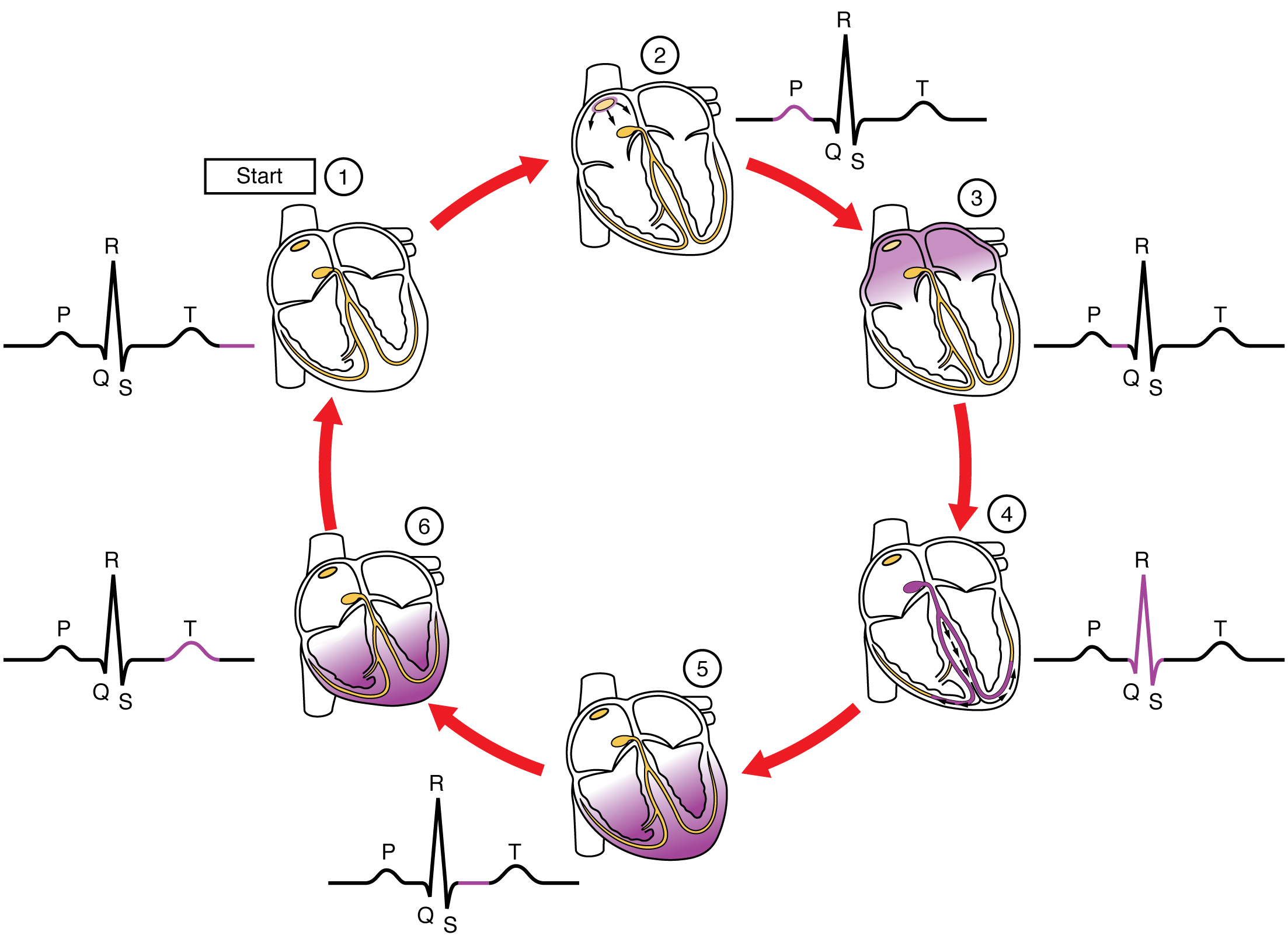
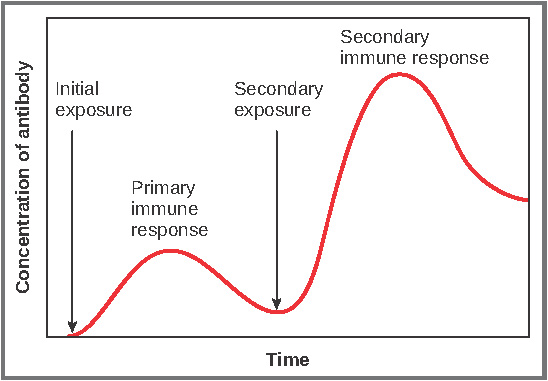
We can detect and record the electrical activity of the heart’s conduction system using an electrocardiogram (ECG or EKG). Figure 12.7 shows the electrical impulse originating in the SA node (step 2) and travelling through the heart’s conduction system, allowing the heart to complete one cardiac cycle. Each waveform on the ECG tracing represents electricity moving through and affecting a different part of the heart. Did you notice that the AV valves close when the electrical impulse reaches the ventricles, just before systole occurs?
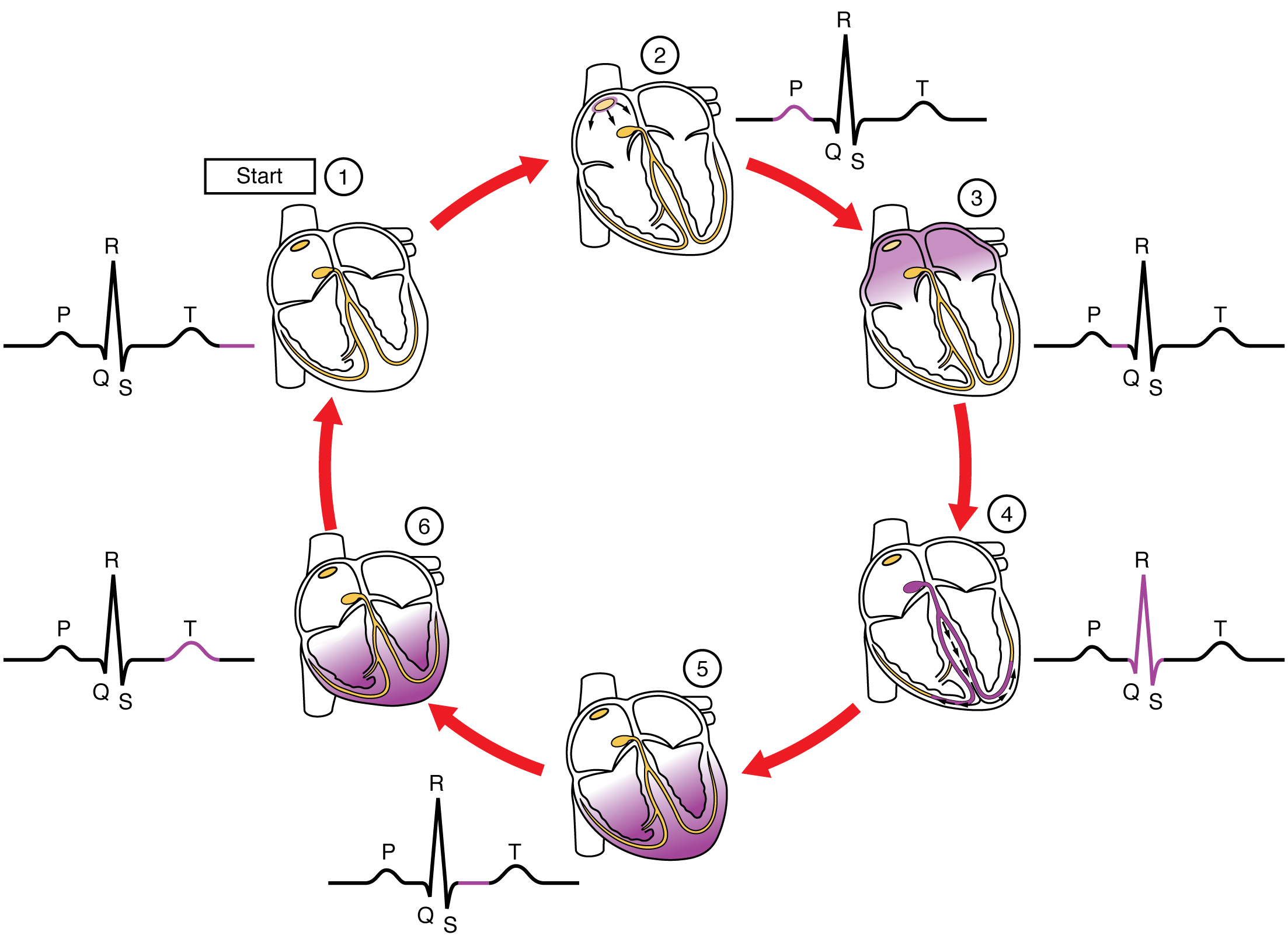
Figure 12.7. ECG Tracing Correlated to the Cardiac Cycle. This diagram correlates an ECG tracing with the electrical and mechanical events of a heart contraction. Each segment of an ECG tracing corresponds to one event in the cardiac cycle. From Betts, et al., 2013. Licensed under
CC BY 4.0.
[Image description.]Heart Terms not Easily Broken into Word Parts An interactive or media element has been excluded from this version of the text. You can view it online here:
https://ecampusontario.pressbooks.pub/medicalterminology/?p=259
Heart Abbreviations
Many terms and phrases related to the cardiovascular system- heart are abbreviated.
Learn these common abbreviations by expanding the list below.
An interactive or media element has been excluded from this version of the text. You can view it online here:
https://ecampusontario.pressbooks.pub/medicalterminology/?p=259
Diseases and Disorders
Cardiomyopathy
The heart of a well-trained athlete can be considerably larger than the average person’s heart. This is because exercise results in an increase in muscle cells called hypertrophy . Hearts of athletes can pump blood more effectively at lower rates than those of non-athletes. However, when an enlarged heart is not the result of exercise, it may be due to hypertrophic cardiomyopathy. The cause of an abnormally enlarged heart muscle is unknown, but the condition is often undiagnosed and can cause sudden death in apparently otherwise healthy young people (Betts, et al., 2013).
Other types of cardiomyopathy include:
- Dilated cardiomyopathy, which also has an unknown cause and is seen in people of any age. In this disorder, one of the ventricles of the heart is larger than normal.
- Arrhythmogenic cardiomyopathy, an inherited condition which results in irregular heart rhythms.
- Restrictive cardiomyopathy, which is a complication of other conditions which cause the myocardium to scar or stiffen (Centers for Disease Control and Prevention, 2019).
Cardiomyopathy may also be caused by myocardial infarctions, myocardial infections, pregnancy, alcohol or cocaine abuse, autoimmune and endocrine diseases. Because the myocardium is responsible for contracting and pumping blood, patients with cardiomyopathy experience impaired heart function which may lead to heart failure. (Centers for Disease Control and Prevention, 2019). To learn more about cardiomyopathy visit the CDC’s cardiomyopathy web page.
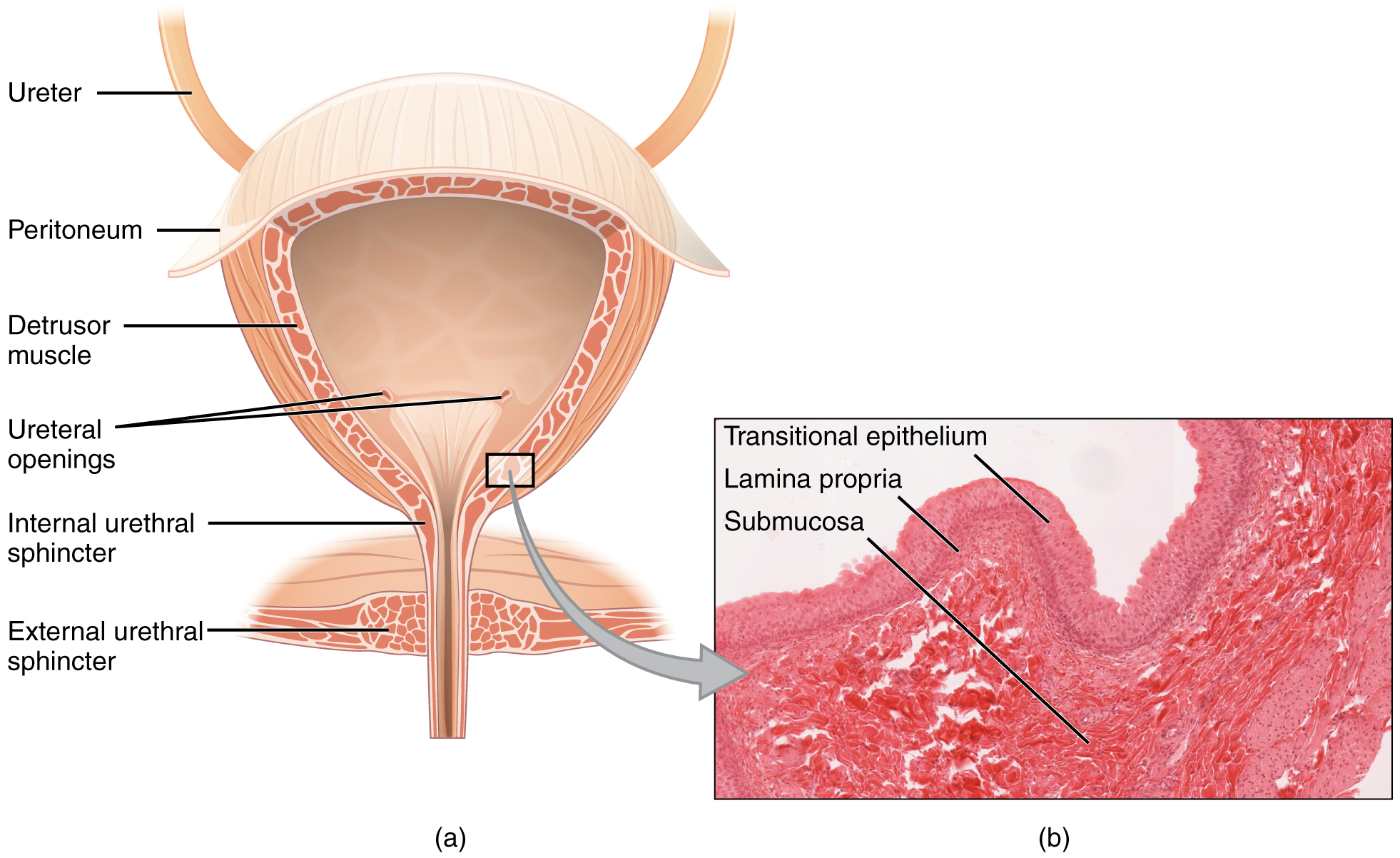
Heart Failure
Heart failure is defined as the inability of the heart to pump enough blood to meet the needs of the body. It is also called congestive heart failure (CHF). This condition causes swelling in the lower extremities and shortness of breath, due to a buildup of fluid in the lungs. It may be caused by cardiomyopathy and it may lead to hypertension and heart valve disorders (Heart & Stroke, n.d.). To learn more, visit the Heart & Stroke’s congestive heart failure web page.
Valvular Heart Disease
The four heart valves open and close at specific times during the cardiac cycle, in order to ensure that blood flows in only one direction through the heart. This requires that these valves open and close completely. Infections such as rheumatic disease or bacterial endocarditis can affect the heart valves and result in scar tissue formation which interferes with valve function. Other causes of heart valve disease include: congenitally malformed valves, autoimmune diseases, and other cardiovascular diseases such as aortic aneurysms and atherosclerosis (Centers for Disease Control and Prevention, 2019a).
Heart valve disease may be asymptomatic, or cause dyspnea, arrhythmias, fatigue and other symptoms. It is often detected when a heart murmur is heard through a stethoscope (Centers for Disease Control and Prevention, 2019a).
- Mitral Valve Prolaspse
- The mitral (bicuspid) valve is diseased or malformed and is not able to close completely, allowing the regurgitation of blood back into the left atrium during systole. Because some of the blood goes back into the atrium, insufficient blood is pumped out of the ventricle into the systemic circulation. This inability to close properly and the resulting regurgitation may also be found in other heart valves (Centers for Disease Control and Prevention, 2019a).
- Aortic Stenosis
- The aortic valve is narrowed and hardened, preventing it from opening fully and allowing sufficient blood to travel to the systemic circulation. Any heart valve can be stenosed, but this disorder most often affects the aortic valve (Centers for Disease Control and Prevention, 2019a).
Visit the CDC’s page on valvular heart disease to learn more.
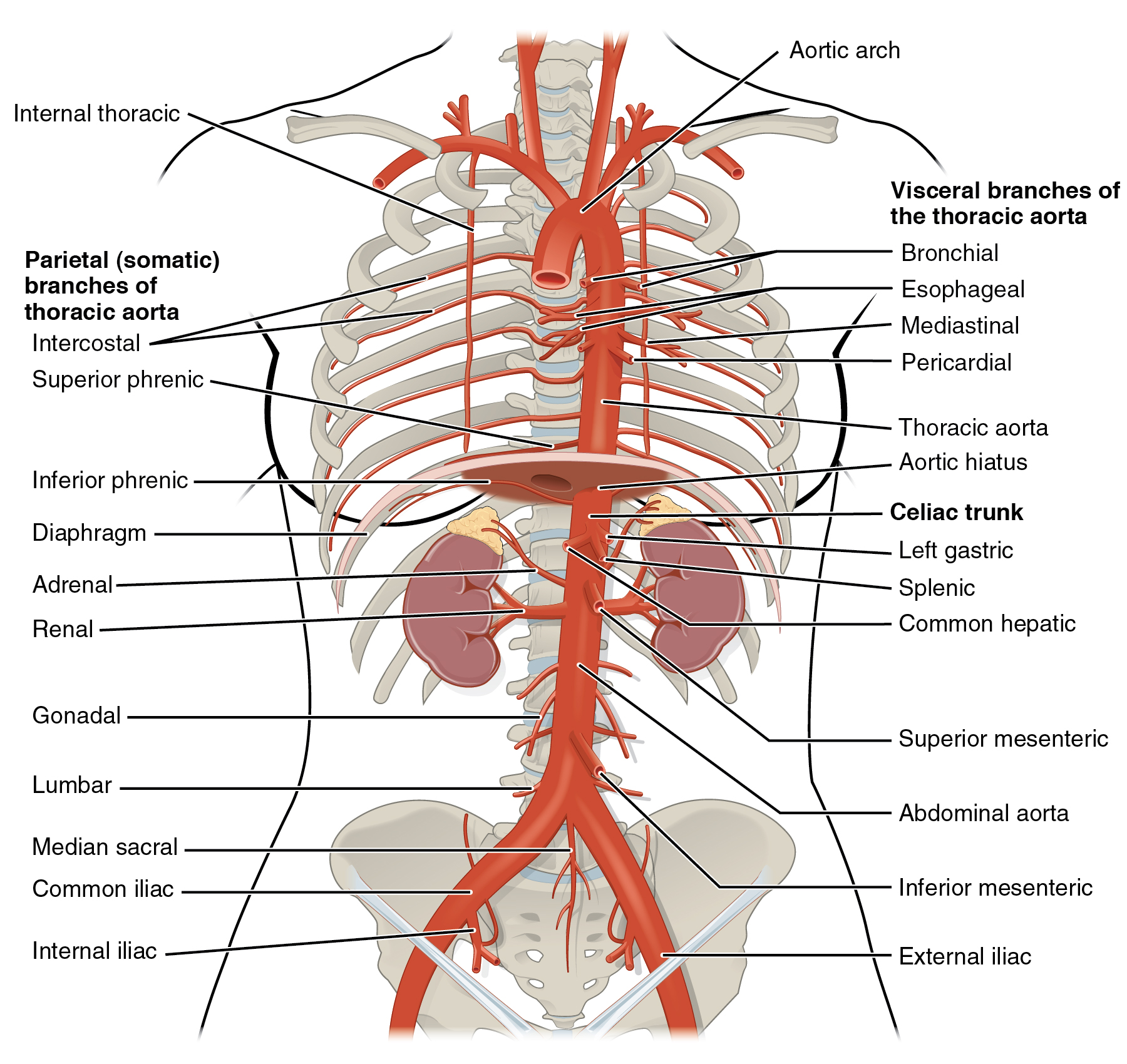
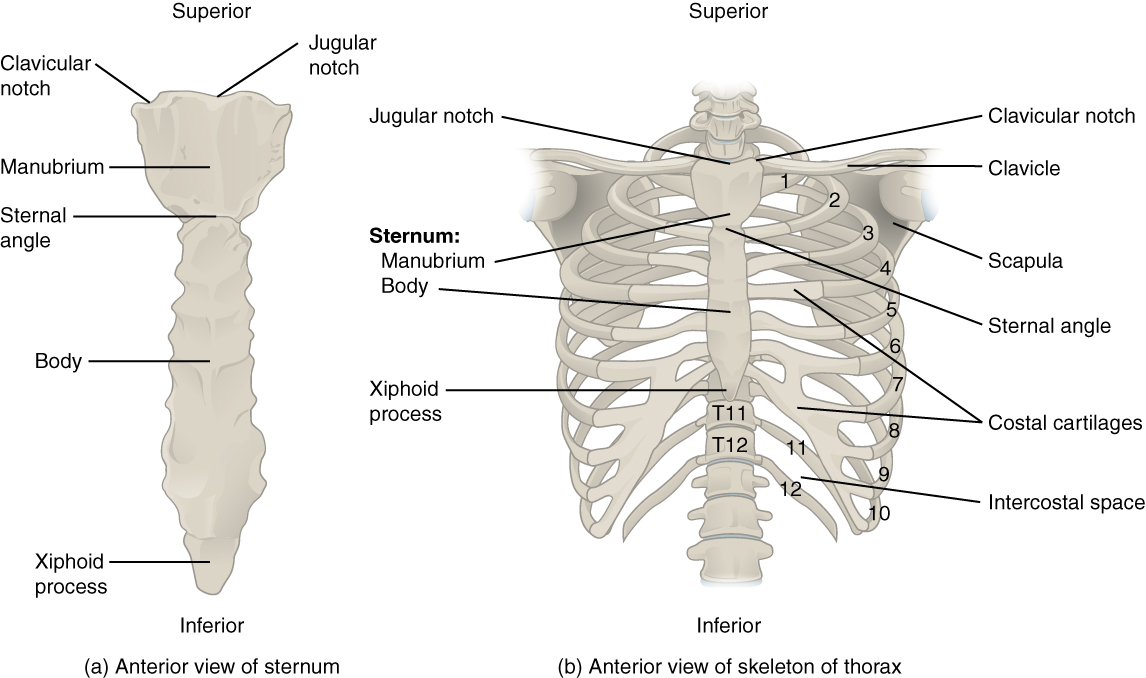
Aneurysms
An aneurysm is a defect in the wall of an artery in which the wall becomes thin and weak and starts to balloon out as blood pulses against the vessel wall. This can happen to any artery and even to the myocardial walls. Aneurysms sometimes occur in the portion of the aorta that is in the thorax (see Figure 12.8). If these aneurysms start to leak between layers of the vessel wall, the condition is known as aortic dissection. If an aortic or cardiac aneurysm bursts, there is sudden, massive internal bleeding (Centers for Disease Control and Prevention, 2019b).
People who smoke, have hypertension, hypercholesterolemia, and/or atherosclerosis have an increased risk of developing aneurysms. Having a family history of aneurysms or certain genetic diseases may also increase a person’s risk of developing an aneurysm.
Aneurysms are often asymptomatic and may be detected incidentally during diagnostic tests that are being done for other reasons. They are sometimes repaired surgically and sometimes treated with medications such as antihypertensives (Centers for Disease Control and Prevention, 2019b; Tittley, n.d.). Visit the Canadian Society for Vascular Surgery’s page on thoracic aortic aneurysms to learn more.
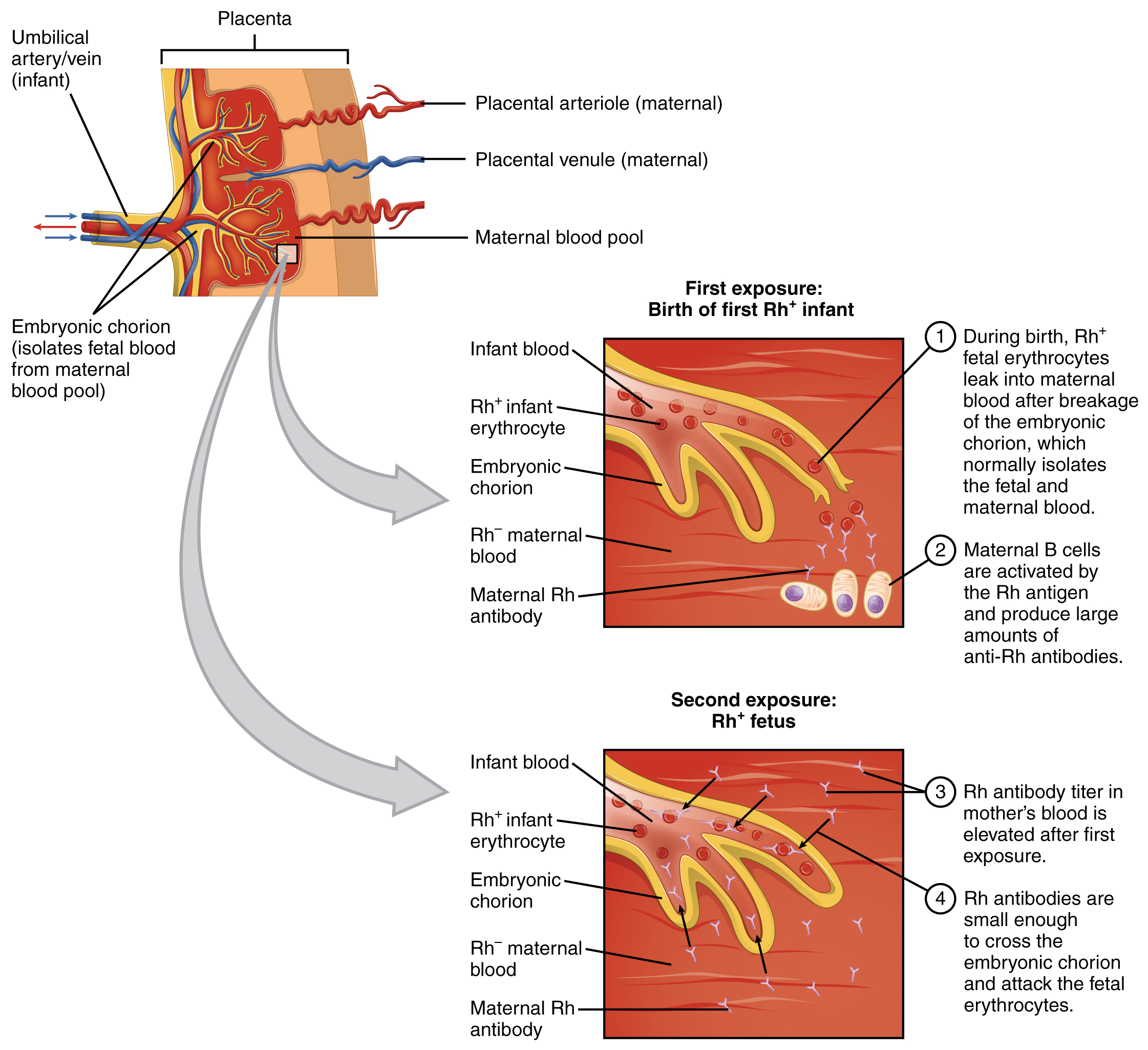
Heart Defects
Fetal circulation is different from postnatal circulation. There are 2 extra openings in the fetal heart, the foramen ovale and the ductus arteriosus, which allow blood circulation that bypasses the immature fetal lungs. The fetal blood is reoxygenated by the mother’s lungs and transported between mother and fetus via the placenta. These two openings usually close around the time of birth (Betts, et al., 2013).
Septal defects are commonly first detected through auscultation. Unusual heart sounds may be detected because blood is not flowing and valves are not closing correctly. Medical imaging is ordered to confirm or rule out a diagnosis. In many cases, treatment may not be needed.
- Patent ductus arteriosus is a congenital condition in which the ductus arteriosus fails to close. If untreated, the condition can result in congestive heart failure.
- Patent foramen ovale is one type of atrial septal defect (ASD), due to a failure of the hole in the interatrial septum to close at birth.
- As much as 20 – 25 percent of the general population may have a patent foramen ovale, most have the benign, asymptomatic version but in extreme cases a surgical repair is required to close the opening permanently.
- Tetralogy of Fallot is a congenital condition that may also occur from exposure to unknown environmental factors; it occurs when there is an opening in the interventricular septum caused by blockage of the pulmonary trunk, normally at the pulmonary semilunar valve. This allows blood that is relatively low in oxygen from the right ventricle to flow into the left ventricle and mix with the blood that is relatively high in oxygen.
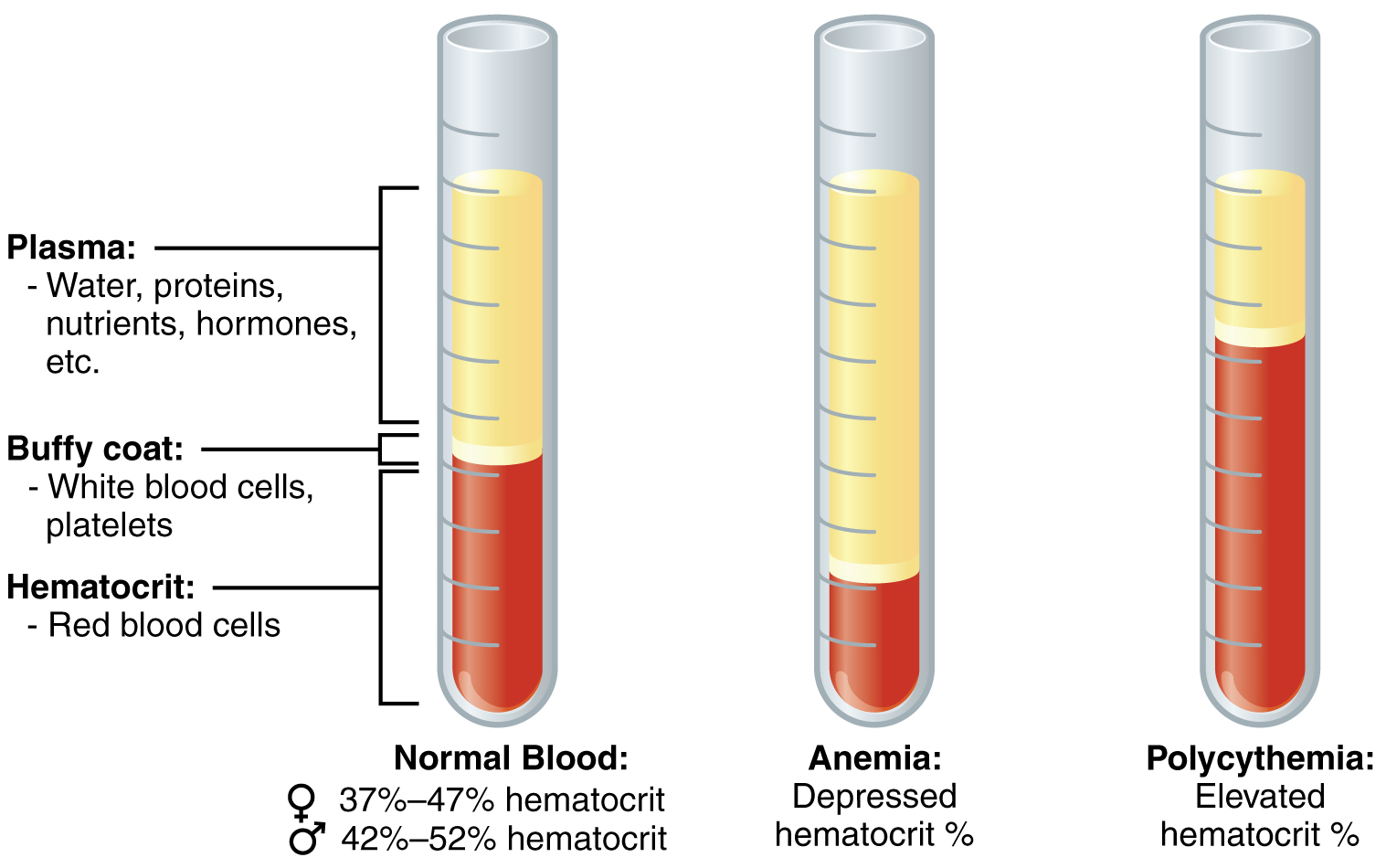
- Symptoms include a distinct heart murmur, low blood oxygen percent saturation, dyspnea, polycythemia, clubbing of the fingers and toes, and in children, difficulty in feeding or failure to grow and develop.
- It is the most common cause of cyanosis following birth. Other heart defects may also accompany this condition, which is typically confirmed by echocardiography imaging.
- In the case of severe septal defects, including both tetralogy of fallot and patent foramen ovale, failure of the heart to develop properly can lead to a condition commonly known as a blue baby Regardless of normal skin pigmentation, individuals with this condition have an insufficient supply of oxygenated blood, which leads to cyanosis, especially when active (Betts, et al., 2013).

Figure 12.9. Congenital Heart Defects. (a) A patent foramen ovale defect is an abnormal opening in the interatrial septum, or more commonly, a failure of the foramen ovale to close. (b) Coarctation of the aorta is an abnormal narrowing of the aorta. (c) A patent ductus arteriosus is the failure of the ductus arteriosus to close. (d) Tetralogy of Fallot includes an abnormal opening in the interventricular septum. From Betts, et al., 2013. Licensed under
CC BY 4.0.
[Image description.]Diseases of the Coronary Circulation
Coronary Artery Disease (CAD)
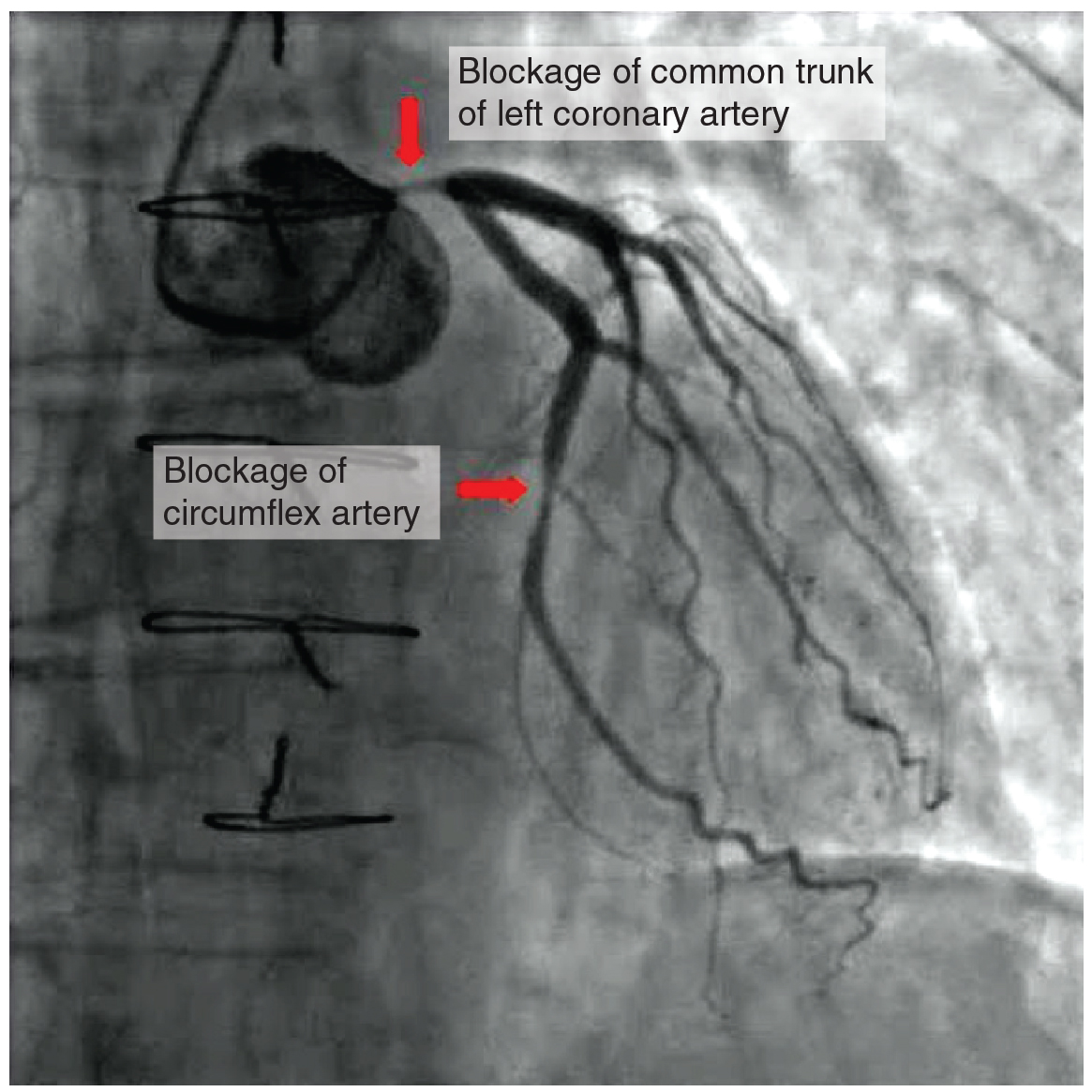
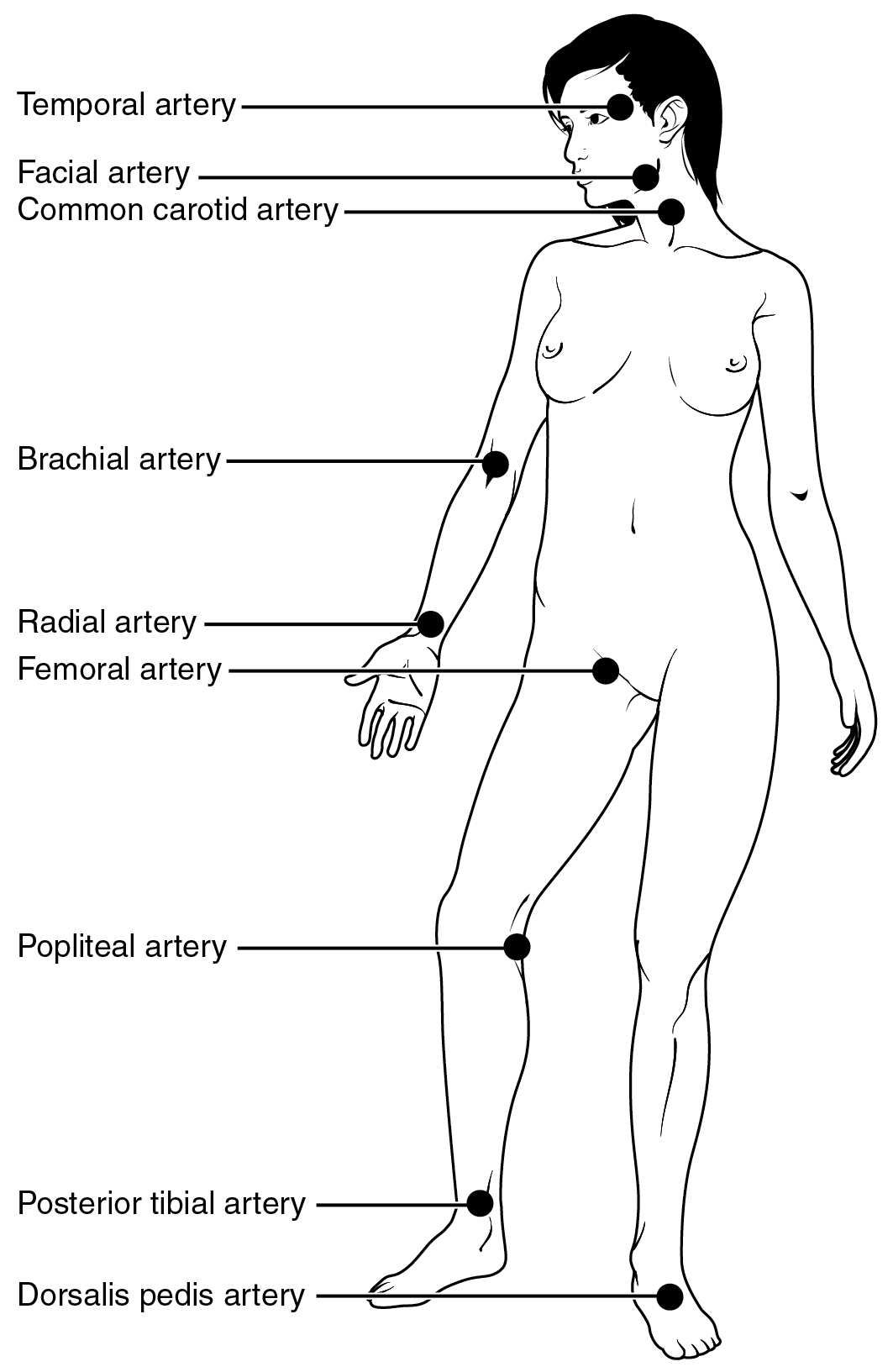
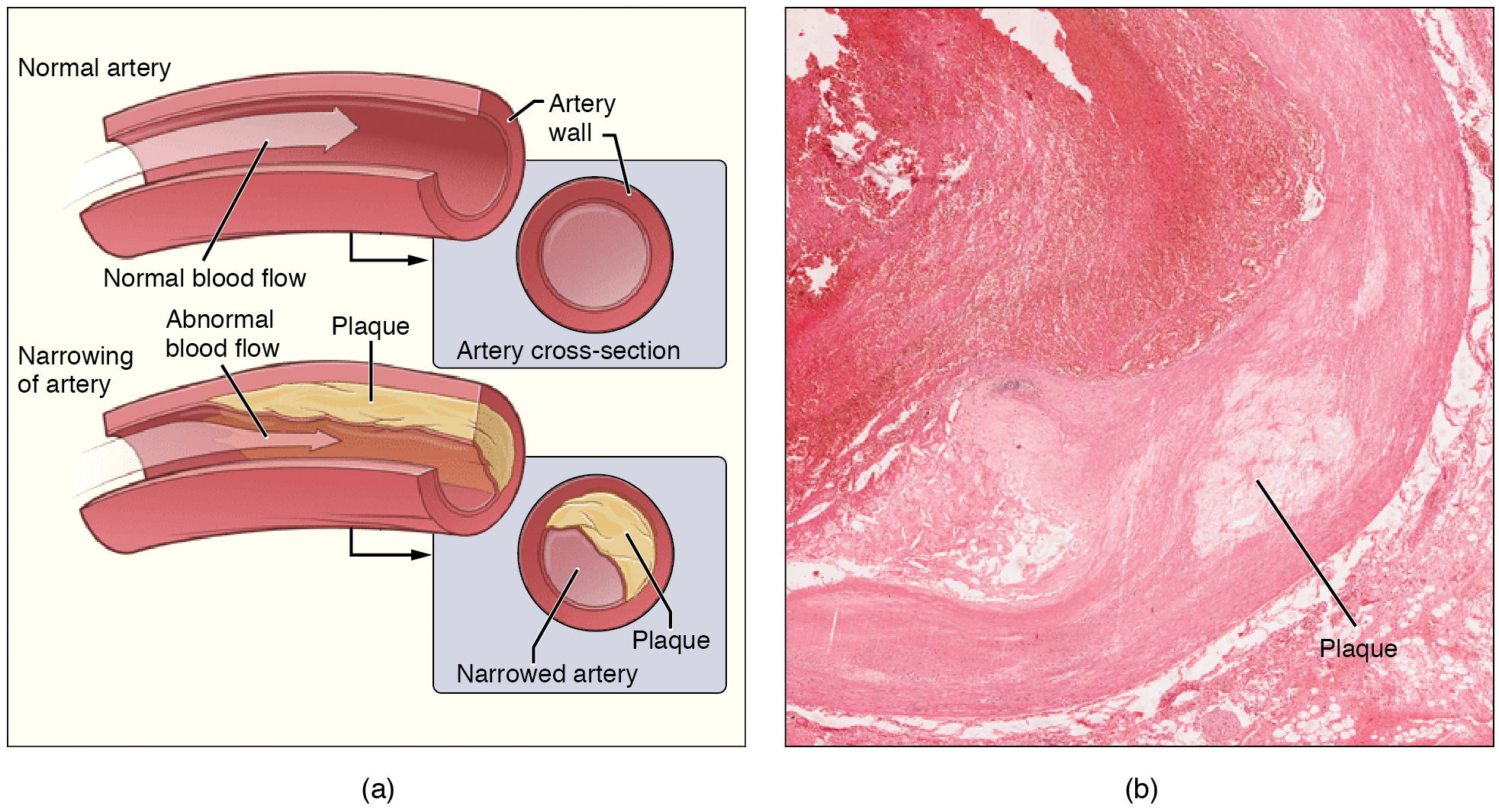
Coronary artery disease occurs when the buildup of plaque in the coronary arteries obstructs the flow of blood and decreases compliance of the vessels. This condition is called atherosclerosis. As the disease progresses and coronary blood vessels become more and more narrow, cells of the myocardium become ischemic, which causes symptoms of angina pectoris, in some patients. If untreated, coronary artery disease can lead to MI.
The image below shows the blockage of coronary arteries on an angiogram (Betts, et al., 2013).
CAD is progressive and chronic. Risk factors include smoking, family history, hypertension, obesity, diabetes, high alcohol consumption, lack of exercise, stress, and hyperlipidemia. Treatments may include medication, changes to diet and exercise, angioplasty with a balloon catheter, insertion of a stent, or coronary artery bypass graft (CABG) (Betts, et al., 2013).
- Angioplasty is a procedure in which the occlusion is mechanically widened with a balloon. A specialized catheter with an expandable tip is inserted into a blood vessel in the arm or leg, and then directed to the site of the occlusion. At this point, the balloon is inflated to compress the plaque material and to open the vessel to increase blood flow. Once the balloon is deflated and retracted, a stent consisting of a specialized mesh is typically inserted at the site of occlusion to reinforce the weakened and damaged walls and prevent re-occlusion.
- Coronary bypass surgery (Coronary artery bypass graft CABG) is a surgical procedure which grafts a replacement vessel obtained from another part of the body to bypass the occluded area. (Betts, et al., 2013).
Myocardial Infarction
Myocardial infarction (MI) is the medical term for a heart attack.
An MI normally results from a lack of blood flow to a region of the heart, resulting in death of the cardiac muscle cells. An MI often occurs when a coronary artery is blocked by the buildup of atherosclerotic plaque. It can also occur when a piece of an atherosclerotic plaque breaks off and travels through the coronary arterial system until it lodges in one of the smaller vessels. MIs may be triggered by excessive exercise, in which the partially occluded artery is no longer able to pump sufficient quantities of blood, or severe stress, which may induce spasm of the smooth muscle in the walls of the vessel (Betts, et al., 2013).
In the case of acute MI (AMI), there is often sudden pain beneath the sternum (retrosternal pain) called angina pectoris, often radiating down the left arm in males but not in female patients. Other common symptoms include dyspnea, palpitations, nausea and vomiting, diaphoresis, anxiety, and syncope. Many of the symptoms are shared with other medical conditions, including anxiety attacks and simple indigestion, so differential diagnosis is critical (Betts, et al., 2013).
An MI can be confirmed by examining the patient’s ECG.
Other diagnostic tests include:
- echocardiography.
- CT.
- MRI.
- Common blood tests indicating an MI include elevated levels of creatine kinase MB and cardiac troponin, both of which are released by damaged cardiac muscle cells (Betts, et al., 2013).
MIs may induce dangerous heart rhythms and even cardiac arrest. Important risk factors for MI include coronary artery disease, age, smoking, high blood levels of LDL, low levels of HDL, hypertension, diabetes mellitus, obesity, lack of physical exercise, chronic kidney disease, excessive alcohol consumption, and use of illegal drugs (Betts, et al., 2013).
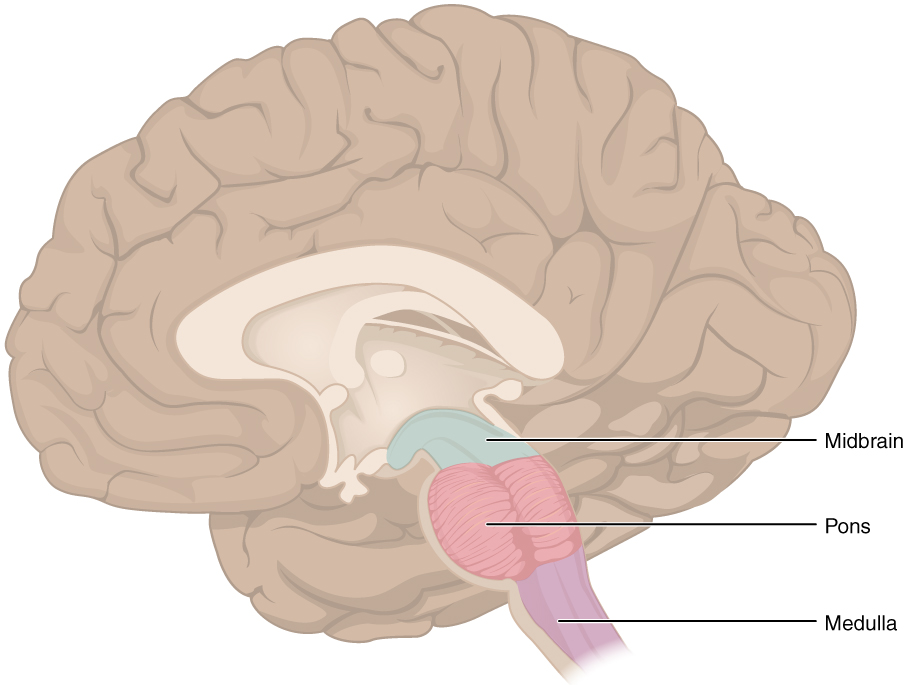
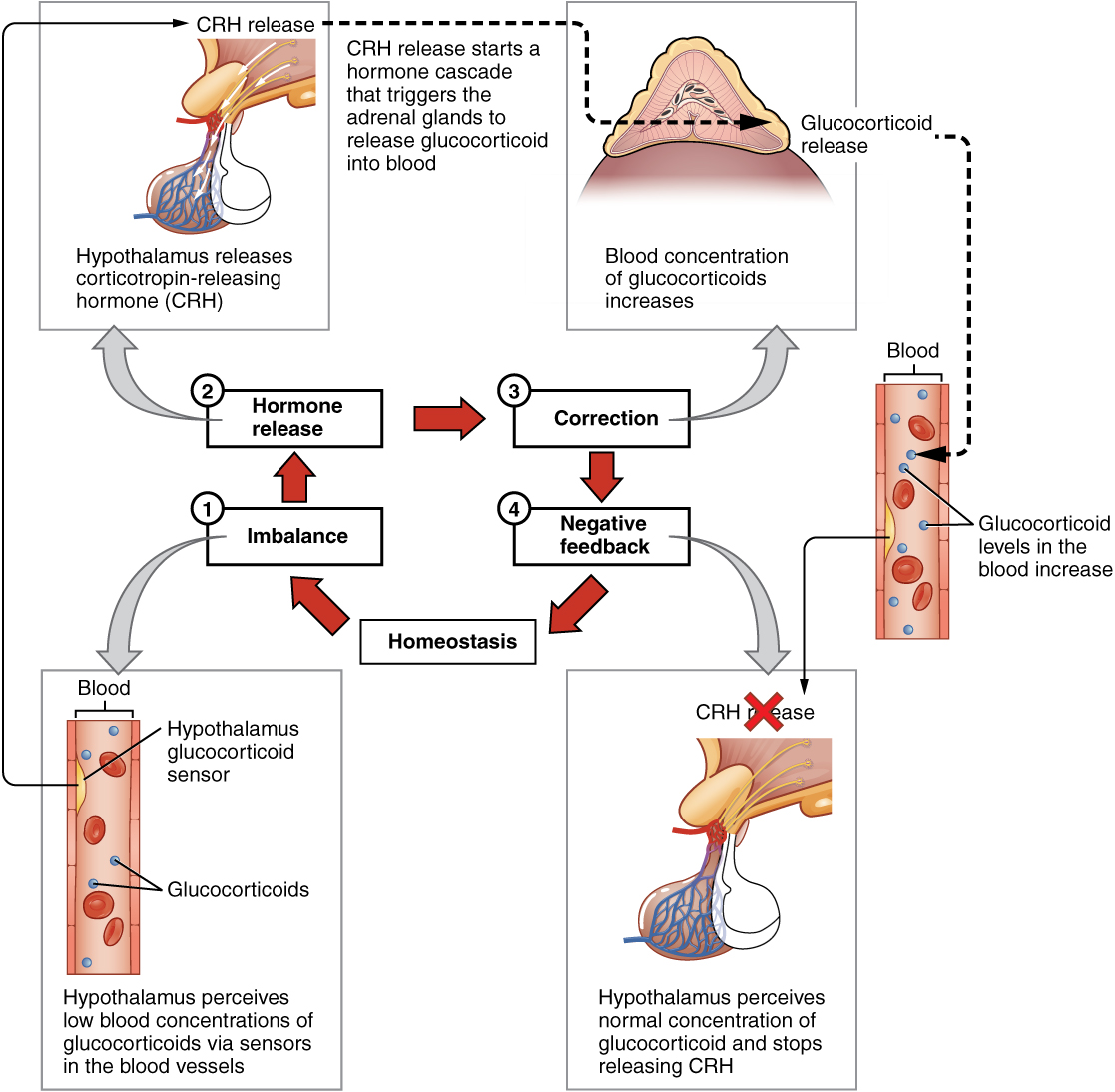
Diseases of the (Electrical) Conduction System
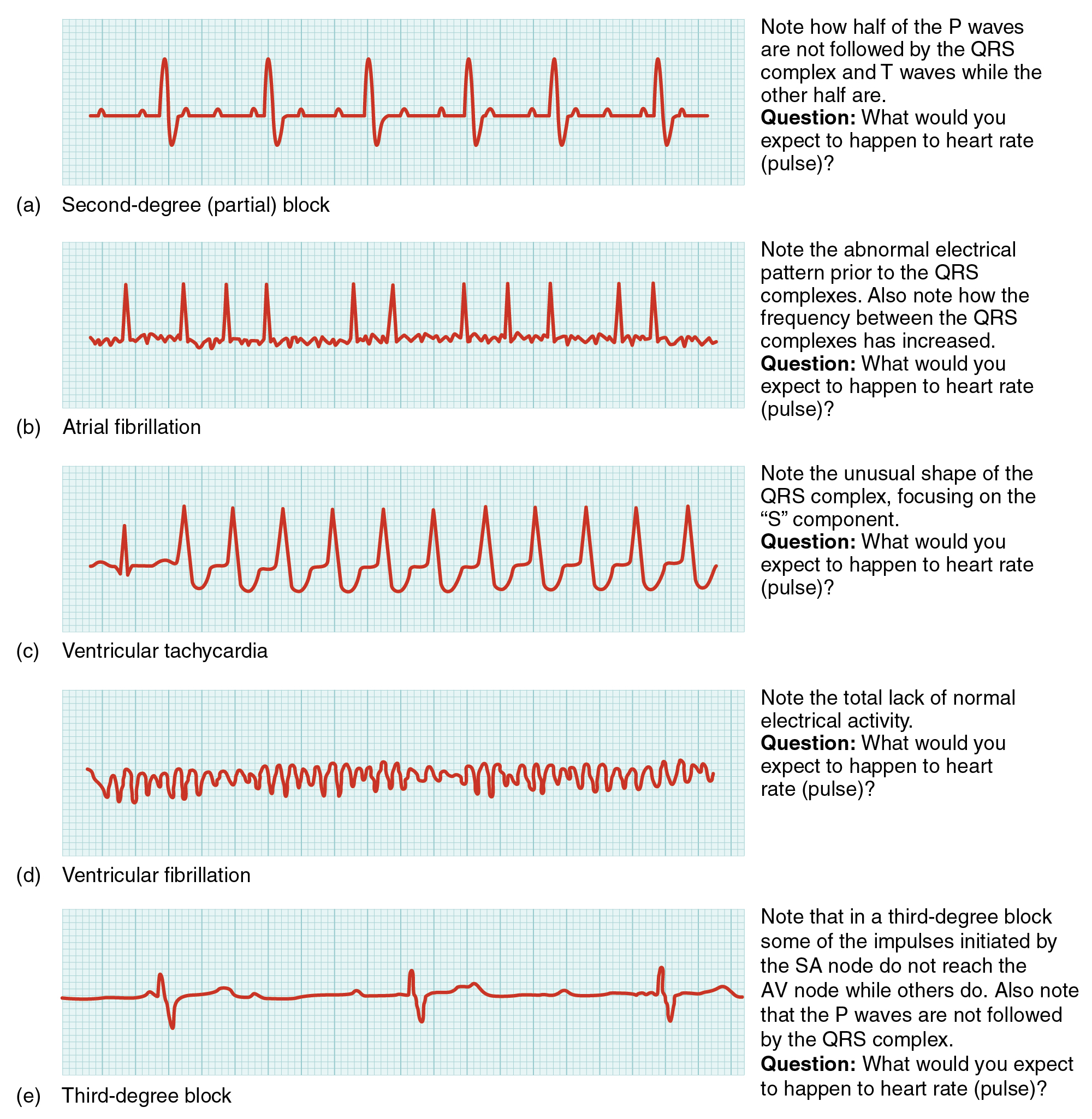
Arrhythmia
The heart’s natural pacemaker, the sinoatrial (SA) node initiates an electrical impulse 60-90 times per minute in a resting adult. This impulse travels through the heart’s conduction system in order to ensure a smooth, coordinated pumping action. This electrical activity can be detected and recorded through the skin using an electrocardiograph. Arrhyhmias may occur when the SA node fails to initiate an impulse, or when the conduction system fails to transmit that impulse through the heart.
In the event that the electrical activity of the heart is severely disrupted, cessation of electrical activity or fibrillation may occur. In fibrillation, the heart beats in a wild, uncontrolled manner, which prevents it from being able to pump effectively.
- Atrial fibrillation is a serious condition, but as long as the ventricles continue to pump blood, the patient’s life may not be in immediate danger.
- Ventrical fibrillation is a medical emergency that requires life support, because the ventricles are not effectively pumping blood, left untreated ventricular fibrillation may lead to brain death.
The most common treatment is defibrillation which uses special paddles to apply a charge to the heart from an external electrical source in an attempt to establish a normal sinus rhythm. A defibrillator effectively stops the heart so that the SA node can trigger a normal conduction cycle. External automated defibrillators (EADs) are being placed in areas frequented by large numbers of people, such as schools, restaurants, and airports. These devices contain simple and direct verbal instructions that can be followed by non-medical personnel in an attempt to save a life (Betts, et al., 2013).
Abnormal Heart Rates
Bradycardia is the condition in which resting adult heart rate drops below 60 bpm. a client exhibiting symptoms such as weakness, fatigue, dizziness, syncope, chest discomfort, palpitations or respiratory distress may indicate that the heart is not providing sufficient oxygenated blood to the tissues. If the patient is not exhibiting symptoms then bradycardia is not considered clinically significant. The term relative bradycardia may be used with a patient who has a HR in the normal range but is still suffering from these symptoms. Most patients remain asymptomatic as long as the HR remains above 50 bpm.
Tachycardia is the condition in which the resting rate is above 100 bpm. Tachycardia is not normal in a resting patient and may be detected in pregnant women or individuals experiencing extreme stress. Some individuals may remain asymptomatic, but when present, symptoms may include dizziness, shortness of breath, rapid pulse, heart palpitations, chest pain, or syncope. Treatment depends upon the underlying cause but may include medications, implantable cardioverter defibrillators, ablation, or surgery (Betts, et al., 2013).
Heart Block
A heart block refers to an interruption in the normal conduction pathway. Heart blocks are generally named after the part of the conduction system that is causing the problem. For example, bundle branch blocks occur within either the left or right atrioventricular bundle branches.
AV blocks are often described by degrees. A first-degree or partial block indicates a delay in conduction between the SA and AV nodes. A second-degree or incomplete block occurs when some impulses from the SA node reach the AV node and continue, while others do not. In the third-degree or complete block, there is no correlation between atrial activity and ventricular activity. This means that none of the impulses generated by the SA node get transmitted to the rest of the heart and the AV node must take over as the primary pacemaker, initiating contractions at 40–60 beats per minute, which is adequate to maintain consciousness.
In order to speed up the heart rate and restore full sinus rhythm, a cardiologist can implant an artificial pacemaker, which delivers electrical impulses to the heart muscle to ensure that the heart continues to contract and pump blood effectively. These artificial pacemakers are programmable by the cardiologists and can either provide stimulation temporarily upon demand or on a continuous basis. Some devices also contain built-in defibrillators (Betts, et al., 2013).
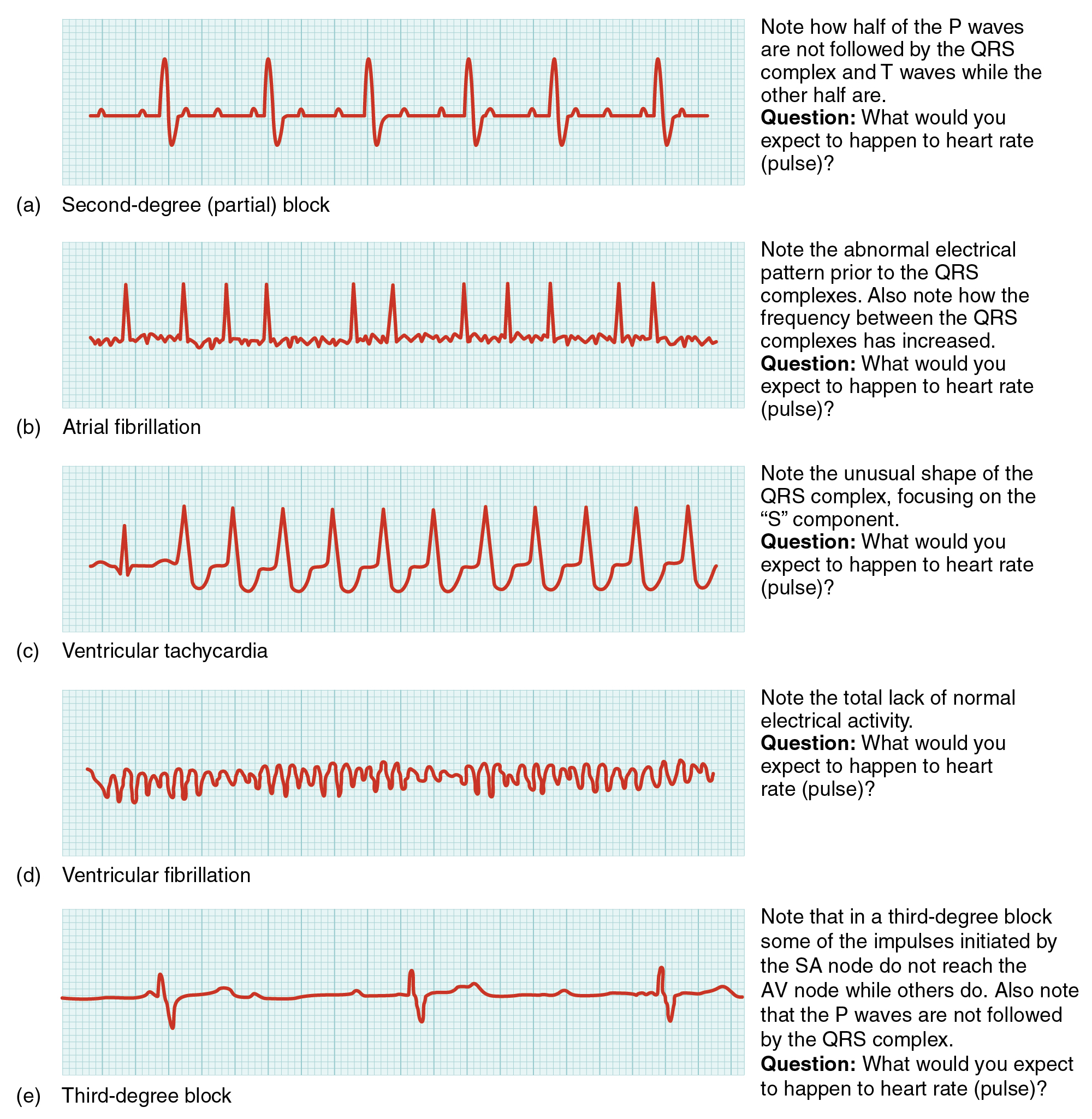
Figure 12.11. Common ECG Abnormalities. (a) In a second-degree or partial block, one-half of the P waves are not followed by the QRS complex and T waves while the other half are. (b) In atrial fibrillation, the electrical pattern is abnormal prior to the QRS complex, and the frequency between the QRS complexes has increased. (c) In ventricular tachycardia, the shape of the QRS complex is abnormal. (d) In ventricular fibrillation, there is no normal electrical activity. (e) In a third-degree block, there is no correlation between atrial activity (the P wave) and ventricular activity (the QRS complex). From Betts, et al., 2013. Licensed under
CC BY 4.0.
[Image description.]Medical Terms in Context
An interactive or media element has been excluded from this version of the text. You can view it online here:
https://ecampusontario.pressbooks.pub/medicalterminology/?p=259
Medical Specialties and Procedures Related to the Heart
Cardiologists and Cardiovascular Surgeons
Cardiologists are medical doctors that specialize in diagnosing and treating heart disease non-invasively. Cardiovascular/thoracic surgeons provide surgical treatments for the heart and other thoracic organs (Canadian Medical Association, 2018). To learn more about these specialists please visit the CMA’s Canadian Specialy Profiles web page.
Cardiology Technologists
Cardiology Technologists complete a college training program and perform diagnostic tests such as electrocardiography, stress testing, Holter monitor testing, ambulatory blood pressure testing, as well as pacemaker monitoring and programming (Canadian Society of Cardiology Technologists, n.d.). Please visit the Canadian Society of Cardiology Technologists web page for more information.
Cardiovascular Perfusionists
Cardiovascular perfusionists complete a college training program and are responsible for operation of the heart-lung bypass machine during open heart surgery. They also monitor the patient’s vitals, adminstering IV fluids, and other drugs (Michener Institute of Education, n.d.). Please visit the Michener Institute’s Cardiovasular Perfusion program page for more information.
Cardiovascular System – Heart Vocabulary
5.25 liters of blood
The volume of blood ejected by the ventricle in one minute is called the cardiac output.
70 mL blood per contraction
The amount of blood ejected from the ventricle in one contraction is called the stroke volume.
Ablation
Using extreme heat or extreme cold to destroy cells in part of the heart which were causing abnormal rhythms.
Angina Pectoris
Chest pain.
Angiogram
An x-ray of the coronary blood vessels using a special catheter and an injection of dye.
Antihypertensives
Class of medications used to treat high blood pressure.
Arrhythmias
Absence of a regular heart rhythm.
Asymptomatic
Pertaining to without symptoms.
Atherosclerosis
A hardening of the arteries that involves the accumulation of plaque.
Auscultation
Listening to the heart using a stethoscope.
AV
Atrioventricular: the area of the heart where the atria and ventricles meet.
AV Valves
Atrioventricular valves: mitral (bicuspid) valve allows blood to flow from left atrium to left ventricle, tricuspid valve allows blood to flow from right atrium to right ventricle.
Bradycardia
Pertaining to a slow heart (rate).
Cardiac Troponin
The regulatory protein for muscle contraction.
Clubbing of the fingers and toes
Broadening of the nails and exaggerated curvature of the nails.
Compliance
The ability of the blood vessels to dilate and constrict as needed.
Congenital
Present at birth.
Creatine Kinase MB
An enzyme that catalyzes the conversion of creatine to phosphocreatine, consuming ATP.
CT
Computerized tomography: a special 3-dimensional x-ray, also called CAT=Computerized Axial Tomography.
Cyanosis
Abnormal condition of blue (bluish colour, lips and nail beds). Typically caused by low oxygenation.
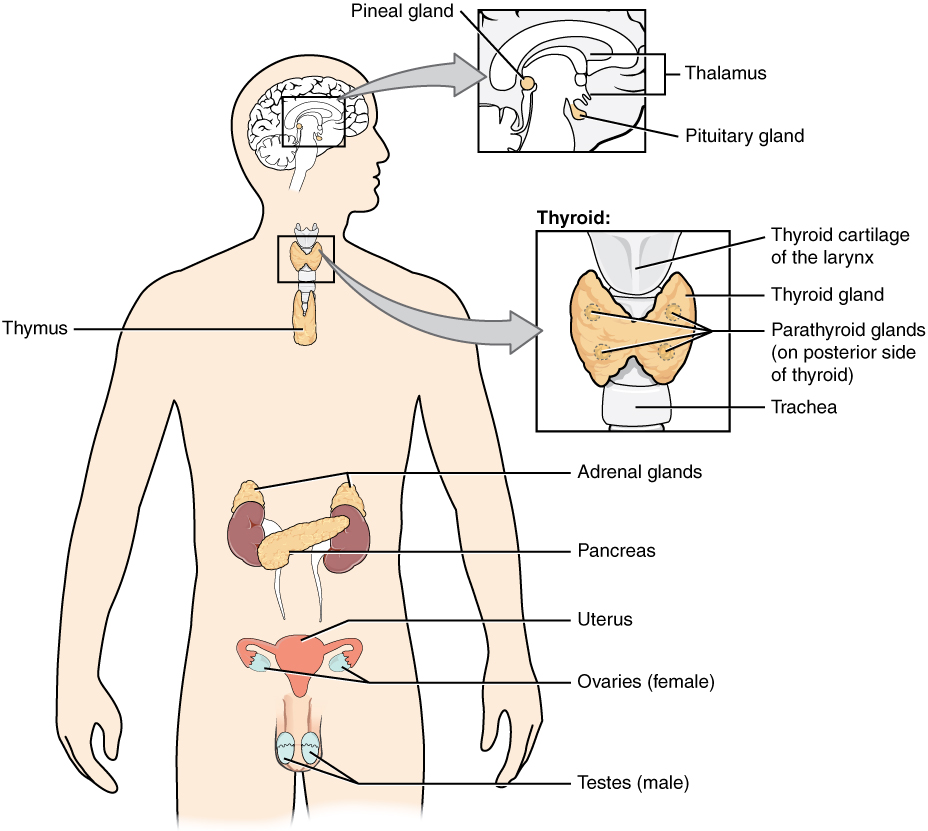
Diabetes Mellitus
An endocrine system disorder in which the pancreas does not produce insulin or the cells of the body do not respond to insulin. This results in high levels of glucose in the blood.
Diaphoresis
Sweating.
Ductus Arteriosus
Connection between pulmonary trunk and aorta in the fetal heart.
Dyspnea
Difficult breathing.
ECG
ECG/EKG both these abbreviations mean electrocardiogram or a recording of the electrical impulses in the heart.
Echocardiography
Process of using sound to record the heart.
Electrocardiograph
Instrument used to record electrical activity within the heart.
Foramen Ovale
Opening between right and left atria, which is normal in the fetal heart.
Great Vessels
The great vessels include the superior vena cava, inferior vena cava, aorta and pulmonary trunk.
HDL
High-density lipoprotein, often referred to as ‘good’ cholesterol.
Heart Murmur
An abnormal heart sound.
Heart Rate
The number of times the heart contracts in one minute.
Hypercholesterolemia
Higher than normal levels of cholesterol in the blood.
Hyperlipidemia
Excessive fat in the blood.
Hypertension
High blood pressure.
Implantable Cardioverter Defibrillators (ICD)
An electronic implant that provides an automatic shock to convert a dangerous heart rhythm to a normal heart rhythm.
Inferior Vena Cava
One of the two largest veins in the body. It carries deoxygenated blood from the torso and legs back to the heart.
Interatrial Septum
The wall separating the right and left atria.
Interventricular Septum
The wall of myocardium that separates the right and left ventricles.
Ischemic
Ischemia is a condition in which cells receive insufficient amounts of blood and oxygen.
LDL
Low-density lipoprotein, often referred to as ‘bad’ cholesterol.
Mitral Valve
Also known as the bicuspid valve.
MRI
Magnetic Resonance Imaging: Highly detailed images produced using a strong magnet and radio waves.
Pacemaker
An electronic implant that initiates a heart beat.
Palpitations
A feeling in the chest that may be caused by an irregular heart rhythm.
Pericardial fluid
Pericardial fluid is a serous fluid which allow the 2 layers of serous pericardium to slide smoothly against each other as the heart beats.
Plaque
A fatty material including cholesterol, connective tissue, white blood cells, and some smooth muscle cells.
Polycythemia
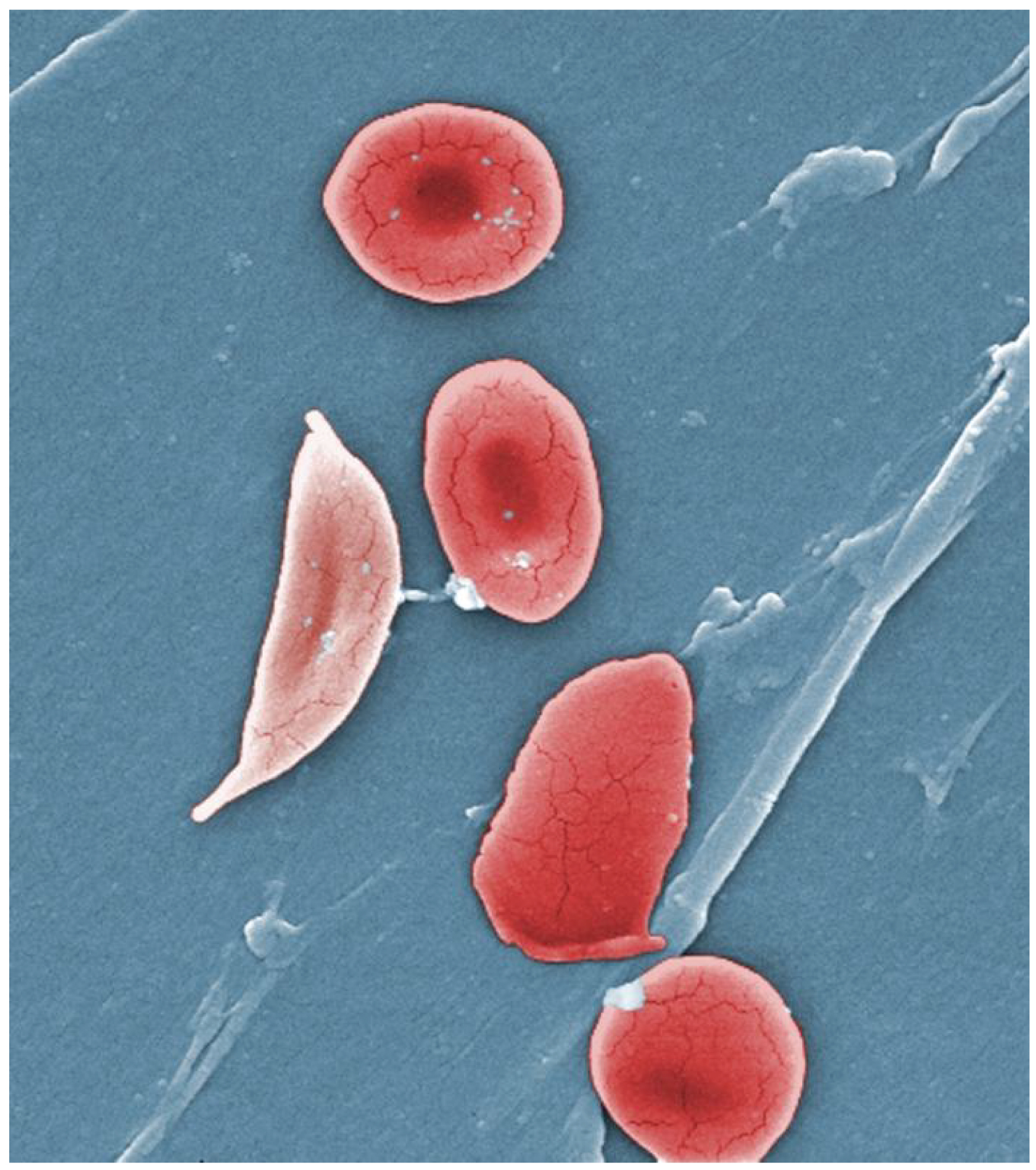
A disorder in which too many red blood cells are produced.
Pulmonary Trunk
Very large artery referred to as a trunk, a term indicating that the vessel gives rise to several smaller arteries.
Roots of the Great Vessels
The part of each great vessel (aorta, pulmonary trunk, inferior vena cava, superior vena cava) that connects to the base of the heart.
Serous
You may recall that serous membranes throughout the body are folded back on themselves, which results in a double-layered membrane separated by serous fluid. The serous membrane surrounding the lungs is called pleura. The serous membrane surrounding the abdominopelvic organs is called peritoneum.
Silent Mis
A myocardial infarction without symptoms. The patient may not know that they are having an MI.
Sinus Rhythm
This is the rhythm set by the heart’s pacemaker, the sinoatrial node and is usually approximately 60-90 beats per minute in a resting adult.
Superior Vena Cava
One of the two largest veins in the body. It carries deoxygenated blood from the head and upper extremities back to the heart.
Syncope
Fainting.
Tachycardia
Condition of a fast heart (rate).
Test Yourself
An interactive or media element has been excluded from this version of the text. You can view it online here:
https://ecampusontario.pressbooks.pub/medicalterminology/?p=259
References
Canadian Medical Association. (2018). Canadian Specialty Profiles. https://www.cma.ca/canadian-specialty-profiles
Canadian Society of Cardiology Technologists. (n.d.). Becoming a registered cardiology technologist. https://www.csct.ca/education/about-being-rct
Centers for Disease Control and Prevention. (2019). Cardiomyopathy. CDC. https://www.cdc.gov/heartdisease/cardiomyopathy.htm
Centers for Disease Control and Prevention. (2019a). Valvular heart disease. CDC. https://www.cdc.gov/heartdisease/valvular_disease.htm
Centers for Disease Control and Prevention. (2019b). Aortic aneurysm. CDC. https://www.cdc.gov/heartdisease/aortic_aneurysm.htm
[CrashCourse]. (2015, July 6). The heart, part 1 – under pressure: Crash course A&P #25 [Video]. YouTube. https://youtu.be/X9ZZ6tcxArI
[CrashCourse]. (2015, July 13). The heart, part 2 – heart throbs: Crash course A&P #26 [Video]. YouTube. https://youtu.be/FLBMwcvOaEo
Heart & Stroke. (n.d.). Heart failure. Heart and Stroke Foundation. https://www.heartandstroke.ca/heart/conditions/heart-failure
Mitchener Institute for Education. (n.d.). Cardiovascular perfusion. Michener Institute of Education at UHN. https://michener.ca/program/cardiovascular-perfusion/
Tittley, J. G. (n.d.). Thoracic aortic aneurysms (TAA). Retrieved from Canadian Society for Vascular Surgery: https://canadianvascular.ca/Thoracic-Aortic-Aneurysms-(TAA)
Image Descriptions
Figure 12.1 image description: This diagram shows the location of the heart in the thorax (sagittal and anterior views). The sagittal view labels read (from top, clockwise): first rib, aortic arch, thoracic arch, esophagus, inferior vena cava, diaphragm, thymus, trachea. The anterior view lables read (from top, clockwise): mediastinum, arch of aorta, pulmonary trunk, left auricle, left lung, left ventricle, pericardial cavity, apex of heart, edge of parietal pericardium, diaphgragm, edge of parietal pleura, ribs, right ventricle, right atrium, right auricle, right lung, superior vena cava. [Return to Figure 12.1].
Figure 12.2 image description: This image shows a magnified view of the structure of the heart wall. Labels read (from top, clockwise): pericardial cavity, fibrous pericardium, parietal layer of serous pericardium, epicardium (visceral layer of serous pericardium), myocardium, endocardium. [Return to Figure 12.2].
Figure 12.3 image description: This diagram shows the network of blood vessels in the lungs. Labels read (from top, clockwise (left-side of the body): aortic arch, pulmonary trunk, left lung, left pulmonary arteries, left pulmonary vein, pulmonary capillaries, descending aorta, (right side of body) inferior vena cava, right pulmonary veins, right pulmonary arteries, right lung, superior vena cava, ascending aorta. [Return to Figure 12.3].
Figure 12.4 image description: The top panel shows the human heart with the arteries and veins labeled (from top, clockwise): aorta, left pulmonary arteries, pulmonary trunk, left atrium, left pulmonary veins, aortic semilunar valve, mitral valve, left ventricle, inferior vena cava, right ventricle, tricuspid valve, right atrium, pulmonary semilunar valve, right pulmonary veins, right pulmonary arteries, superior vena cava. The bottom panel shows a rough map of the the human circulatory system. Labels read (from top, clockwise): systemic capillaries of upper body, systemic arteries to upper body, pulmonary trunk, left atrium, left ventricle, systemic arteries to lower body, systemic capillaries of lower body, systemic veins from lower body, right ventricle, right atrium, pulmonary capillaries in lungs, systemic veins from upper body. [Return to Figure 12.4].
Figure 12.5 image description: The top panel of this figure shows the anterior view of the heart while the bottom panel shows the posterior view of the heart. The different blood vessels are labeled. Anterior view labels (from top of diagram, clockwise): left coronary artery, pulmonary trunk, circumflex artery, anterior interventricular artery, great cardiac vein, small cardiac vein, anterior cardiac veins, atrial arteries, right atrium, right coronary artery, ascending aorta, aortic arch. Posterior view labels (from top of diagram, clockwise): coronary sinus, small cardiac vein, right coronary artery, marginal artery, middle cardiac vein, posterior cardiac vein, posterior interventricular artery, marginal artery, great cardiac vein, circumflex artery. [Return to Figure 12.5].
Figure 12.6 image description: This image shows the anterior view of the frontal section of the heart with the major parts labeled. Labels read (from top of diagram, clockwise) arch of aorta, Bachman’s bundle, atrioventricular bundle (bundle of His), left ventricle, right and left bundle branches, Purkinje fibers, right ventricle, right atrium, posterior intermodal, middle intermodal, atrioventricular node, anterior intermodal, Sinoatrial node. [Return to Figure 12.6].
Figure 12.7 image description: This diagram shows the six different stages of heart contraction and relaxation along with the stages in the QT cycle. [Return to Figure 12.7].
Figure 12.8 image description: This diagram shows the arteries in the thoracic and abdominal cavity. Visceral branches of the thoracic aorta labels (from top): bronchial, esophageal, mediastinal, pericardial, thoracic aorta, aortic hiatus, celiac trunk, left gastric, splenic, common hepatic, superior mesenteric, abdominal aorta, inferior mesenteric, external iliac. Parietal (somatic) branches of thoracic aorta labels (from top): intercostal, superior phrenic, inferior phrenic, diaphragm, adrenal, renal, gonadal, lumbar, medial sacral, common iliac, internal iliac. [Return to Figure 12.8].
Figure 12.9 image description: This diagram shows the structure of the heart with different congenital defects. The top left panel shows patent foramen ovale (label reads foramen ovale fails to close), the top right panel shows coarctation of the aorta (label reads narrow segment of aorta), the bottom left panel shows patent ductus ateriosus (label reads Ductus arteriosus remains open) and the bottom right shows tetralogy of fallot (labels read aorta emerges from both ventricles, interventricular septal defect, enlarged right ventricle, stenosed pulmonary semilunar valve). [Return to Figure 12.9].
Figure 12.11 image description: In this image the QT cycle for different heart conditions are shown. From top to bottom, the arrhythmias shown are second-degree partial block (text reads: Note how half of the P waves are not followed by the QRS complex and T waves while the other half are. Question: what would you expect to happen to heart rate?), atrial fibrillation (text reads: Note the abnormal electric pattern prior to the QRS complexes. Also note how the frequency between the QRS complexes has increased. Question: What t would you expect to happen to heart rate?), ventricular tachycardia (text reads: Note the unusual shape of the QRS complex, focusing on the S component. Question: What would you expect to happen to heart rate?), ventricular fibrillation (text reads: Note the total lack of normal electrical activity. Question: What would you expect to happen to heart rate?), and third degree block (text reads: Note that in a third-degree block some of the impulses initiated by the SA node do not reach the AV node while others do. Also note that the P waves are not followed by the QRS complex. Question: What would you expect to happen to heart rate?). [Return to Figure 12.11].
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.