Untreated dental caries and severe periodontitis in permanent teeth and untreated caries in deciduous teeth are among the most prevalent chronic non-communicable diseases world-wide. Oral diseases can cause pain and discomfort, increase absenteeism from school/work, and reduce quality of life. Untreated dental decay further affects child growth. Both, dental caries and periodontal disease, are behavioral diseases which could be prevented by reducing use of sugar and by good oral hygiene. Dental caries is more common among Indigenous than non-Indigenous communities. Resources in oral health care (e.g. lack of dentists) are scarce in most places in the Circumpolar area. Therefore, the role of nursing personnel is very important in preventing oral diseases. Oral diseases share risk factors with other chronic, non-communicable diseases. Promoting oral health also benefits general health.
Key Terms: oral health, health promotion, general health, quality of life, Indigenous populations
Introduction
The mouth is a part of the body, although its diseases have been treated by dental personnel rather than by general health care workers. This situation was created when dental caries started to become common along with the increased consumption of sugar during the 18th century. Oral diseases are highly prevalent everywhere. They cause pain and discomfort, increase absenteeism from school and/or work, and reduce quality of life.
Oral Health as a Part of General Health, Well-Being and Quality of Life
Untreated caries (active tooth decay) and severe periodontitis (advanced gum disease) in permanent teeth are the most prevalent chronic diseases (global prevalence of 35%) and among the 291 most common diseases and injuries (Marcenes et al., 2013). Untreated caries in primary teeth is almost equally common. Dental caries is caused by certain bacteria (most often streptococcus mutans) in biofilm attached to teeth (Kidd & Fejerskov, 2016). These bacteria form acids when sucrose, other sugars, or redefined starches are present, and can cause dissolution of tooth surface which lead to cavities (tooth decay, caries lesions). If caries lesion is left untreated, it can lead to a serious infection inside the tooth, which can cause a formulation of abscess or tooth loss (Kidd & Fejerskov, 2016). The main cause of periodontal diseases is also certain bacteria in biofilm (Mueller, 2015). If left untreated, infection can destroy the attachment fibers and supporting bone around root surfaces of teeth, and lead to tooth loss (Mueller, 2015).
As described in Table 1, dental caries is more prevalent among Indigenous people than non-Indigenous in the circumpolar region, such as in Alaska (MMWR, 2011), Canada (Schroth et al., 2005), Greenland (Ekstrand & Qvist, 2014), the northern parts of the Nordic countries (Widström et al., 2010), and north-west Russia (Gorbatova et al., 2012).
Table 1. Dental caries experience and severity among 12-year-olds in the countries of the circumpolar region
| Country | Caries experience (DMFT) – whole country1 | Caries experience (DMFT) – northern areas | Severity level of dental caries – whole country6 | Severity level of dental caries – northern areas6 |
| Canada | 1.0 | 9.52 | Very low | Very high |
| Denmark | 0.4 | – | Very low | – |
| Finland | 0.7 | 1.63 | Very low | Low |
| Greenland | 1.7 | – | Low | – |
| Iceland | 1.4 | – | Low | – |
| Norway | 1.7 | 1.83 | Low | Low |
| Russia | 2.5 | 3.24 | Low | Moderate |
| Sweden | 0.8 | 0.93 | Low | Very low |
| United States | 1.2 | 5.55 | Low | High |
DMFT = The mean number of Decayed, Missing or Filled Teeth in permanent dentition
Sources: 1Malmö University, 2016; 2Schroth et al., 2005; 3Widström et al., 2010; 4Gorbatova et al., 2012; 5MMWR, 2011; 6WHO, 2000
Unfortunately, oral health has not improved over the past 25 years. In contrast, the cumulative burden of oral conditions has dramatically increased between 1990 and 2015 throughout the world (Kassebaum et al., 2017). During that period, the number of untreated oral conditions rose from 2.5 billion to 3.5 billion (Kassebaum et al., 2017). Treatment of oral diseases is also expensive. In 2010, the direct treatment costs due to oral diseases worldwide equaled 4.6% of the global health expenditure (Listl et al., 2015).
Total tooth loss has been shown to have a great impact on general health. Compared to dentate people (i.e. persons with teeth), edentulous people (persons without any teeth) consume fewer vegetables and fruits; more foods with less fiber; more cholesterol and saturated fats; and have a lower carotene intake. Moreover, they typically have low plasma vitamin C levels and increased amounts of inflammatory reactants, such as plasma C-reactive protein (Lowe et al., 2003; Okoro et al. 2005). The excessive intake of highly processed high fat and high carbohydrate foods further contributes to obesity and obesity-related diseases, such as insulin resistance, cardiovascular disease, and hyperlipidemia (Te Morenga & Mann, 2012). Tooth loss is strongly associated with impairment of oral health-related quality of life (OHRQoL) (Gerritsen et al., 2010). Having fewer than nine teeth has more impact on OHRQoL than having cancer, hypertension, or allergy (Gerritsen et al., 2010). Having one’s own teeth for as long as possible is important. The prevention of oral diseases in the remaining teeth, i.e. reduction of pain (toothache), as well as functional and esthetic discomfort, will improve the quality of life of the population.
The most common oral diseases, dental caries and periodontal disease, can be considered as behavioral diseases, which means they have the same risk factors for one’s long-term health as other chronic, non-communicable diseases (Sheiham & Watt, 2000). For instance, poor oral health and oral hygiene have been associated with higher levels of cardiovascular diseases (Buhlin et al., 2003); diabetes and hypertension (Fujita et al., 2009); and metabolic syndrome (Kobayashi et al., 2012). A strong association between inflammatory oral diseases (periodontal disease) and the four main non-communicable diseases: diabetes, cancer, cardiovascular diseases, and respiratory diseases, has been confirmed (UN, 2011).
Sugar is the main risk factor for dental caries, which is the most common chronic disease in the world (Sheiham, 1983, 2001; Petersen, 2003a; Moynihan & Petersen, 2004; Marcenes et al., 2013). The intake of free sugars (added sugars) or sugar sweetened beverages is also a determinant of body weight (Te Morenga et al., 2012). High consumption of sugar beverages is associated with metabolic syndrome and type 2 diabetes (Malik et al., 2010).
Smoking is one of the most common risk factors for chronic diseases, a leading cause of preventable deaths (WHO, 2015), and harms nearly every organ of the body (ASH, 2016). It is considered as a major risk factor for poor periodontal health (Stoltenberg et al., 1993; Petersen, 2003b; Edman et al., 2015). Unfavorable health behaviors tend to cluster together. Irregular toothbrushing is related with high consumption of sweets, smoking, and use of alcohol (Rajala et al., 1980; Currie et al., 1989; Honkala et al., 2011).
Prevention of Oral Diseases
The most common oral diseases could be prevented by the adoption of healthy behaviors (Löe, 2000). Removal of dental plaque by tooth brushing twice-a-day has been accepted as an international recommendation for maintaining good oral hygiene and periodontal health (Sheiham, 1970; Löe, 2000; Zimmerman et al., 2015). Dental caries and erosion of the teeth can be prevented by using fluoride toothpaste when brushing (Walsh et al., 2010; CDC, 2014) and restricting the frequency of between-meal sugar consumption (Sheiham, 2001; Perez et al., 2016). A traditionally healthy diet has been rapidly changed among Indigenous populations to the sugar-rich western type diet after sugary products became easily available (Bang & Kristoffersen, 1972).
Relatively stable patterns of tooth brushing are usually established during childhood and adolescence (Kuusela et al., 1996; Åstrøm & Jakobsen, 1998). Thus, family members, especially parents, can play a vital role in encouraging the adoption of regular tooth brushing habits of their children (Honkala et al., 1983).
Utilizing a population strategy rather than a high-risk-group strategy in health promotion has been shown to be the most cost-effective approach to reduce both the prevalence and the severity of the common chronic diseases (Rose, 2001). Health promotion is, thus, based on a community approach. Community development and empowerment draws on existing human and material resources in the community to facilitate self-help, social support, participation, and ownership. The main focus of oral health promotion activities should be targeted towards children, but a population strategy should also target adults. The Oral Health Program of the World Health Organization (WHO) recommends the development of programs for oral health promotion, which highlights implementation of community-based demonstration projects for oral health promotion, along with a special reference to poor and disadvantaged population groups (Petersen, 2009).
Oral Health Services
There is enormous variation in how oral (dental) health services have been organized worldwide (Arjnljot et al., 1985, Chen et al., 1997). There are also big differences in the number of oral health personnel (i.e. dentists, dental hygienists/therapists, dental nurses/assistants) providing these services (please see Table 2). In the Nordic countries, the governments have been mainly responsible for providing oral health services for their citizens, especially for children under 18 years of age, who have had these services free of charge. Full coverage and preventive orientation of these services have been emphasized (Honkala et al., 1991) and the preference for public funding of oral health services continues to be very strong amongst the Nordic countries (Widström et al., 2005). As a result, low caries prevalence has been achieved among the Nordic children (Johansson et al., 2007). It is also a great achievement that the socioeconomic inequalities in the use of oral health services were totally abolished among Finnish children in the 1990’s, 20 years after the Public Health Law was implemented (Honkala et al., 1997). Children from families with the lowest level of education in Finland and in Norway were found to use dental services more frequently than children from families with higher education (Virtanen et al., 2007). In other words, children with the highest need were more frequently receiving the treatment needed in those two counties. This Nordic public health policy clearly reflects the national strategies of targeting the oral health services according to the needs and to reduce inequalities in oral health. However, socioeconomic inequalities still exist among the adults (Johansson et al., 2007; Raittio et al., 2015), especially among older adults (Holm-Pedersen et al., 2005; Vikum et al., 2012).
Table 2. Number and density of dentists (per 1,000 persons) in the countries of the circumpolar region
| Country | Number of practicing dentists | Density of dentists/1,000 |
| Canada1 | 19.334 | 0.57 |
| Denmark1 | 4.244 | 0.75 |
| Finland1 | 3.925 | 0.72 |
| Greenland2 | 30 | 0.54 |
| Iceland1 | 278 | 0.84 |
| Norway1 | 4.434 | 0.85 |
| Russia3 | 29.400 | 0.32 |
| Sweden1 | 7.777 | 0.80 |
| United States1 | 196.400 | 0.61 |
Sources: 1OECD, 2016; 2Ekstrand & Qvist, 2014; 3Eurostat, 2006
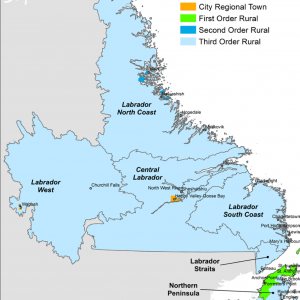
There have been huge difficulties in the northern areas for providing oral health services because of the sparsely distributed vast areas (Abelsen, 2008; Widström et al., 2010). This is especially the case in oral health services in Greenland, Alaska and northern Canada. To address this problem, Alaska established a special school in their capital ten years ago to educate dental health aid therapists by admitting the students from the distant rural areas for being able to get workforce for these regions (ANTHC, 2018). Nevertheless, there continues to be a lack of dental personnel in all the Indigenous regions, not only in Alaska, because dentists prefer to work and live in affluent, typically urban areas. Thus, also other health professionals should participate in oral health promotion, which serves the general health and quality of life of northern communities. International organizations, like the World Dental Federation and the World Health Organization, have published on their webpages toolkits for preventing oral diseases (see Additional Resources). In addition, several national organizations have published online training resources and toolkits for promoting oral health. For example, the Rural Health Information Hub has created an evidence-based toolkit with seven modules, which helps to identify and implement an oral health program in rural communities (RHIhub, 2002-2018). These toolkits can be introduced and promoted amongst local health teams in northern and Indigenous communities to create collective responsibility for oral health promotion, rather than relying on dentists.
Conclusion
Oral health is an important part of general health. Indigenous populations suffer from poor oral health (high prevalence of dental caries) and a shortage of oral health personnel. Therefore, oral health promotion should be emphasized and all health care personnel should support these activities and communities.
References
Abelsen, B. (2008). What a difference a place makes: Dental attendance and self-rated oral health among adults in three counties in Norway. Health & Place 14(4), 827-40.
Action on Smoking and Health (ASH). (2016). Fact sheet: Smoking statistics: Smoking and Disease. Retrieved from: http://ash.org.uk/category/information-and-resources/fact-sheets/
ANTHC, Alaska Native Tribal Health Consortium. (2018). Alaska Dental Therapy Educational Programs. Retrieved from: https://anthc.org/alaska-dental-therapy-education-programs/
Arnljot, H. A., Barmes, D. E., Cohen, L. K., Hunter, P. B. V., & Ship, I. I. (1985). Oral health care systems. An International Collaborative Study. Geneva: World Health Organization.
Åstrøm, A. N., & Jakobsen, R. (1998). Stability of dental health behavior: a 3-year prospective cohort study of 15, 16- and 18-year-old Norwegian adolescents. Community Dentistry & Oral Epidemiology 26(2), 129-38.
Bang, G., & Kristoffersen, T. (1972). Dental caries and diet in an Alaskan Eskimo population. Scandinavian Journal of Dental Research 80(5), 440-4.
Buhlin, K., Gustafsson, A., Håkansson, J., & Klinge, B. (2003). Self-reported oral health, dental care habits and cardiovascular disease in an adult Swedish population. Oral Health & Preventive Dentistry, 1(4), 291-9.
Centers for Disease Control and Prevention (CDC). (2016). Hygiene-related diseases – Dental caries. Atlanta (GA): CDC. Retrieved from: https://www.cdc.gov/healthywater/hygiene/disease/dental_caries.html
Chen, M., Andersen, R. M., Barmes, D. E., Leclercq, M.-H., & Lyttle, C. S. (1997). Comparing oral health care systems. A second international collaborative study. Geneva: World Health Organization.
Currie, C., Schou, L., & McQueen, D.V. (1989). Dental health-related behaviour in Scottish schoolchildren aged 11, 13 and 15 from Edinburgh City. Health Bulletin 47(4), 182-91.
Edman, K., Öhrn, K., Nordström, B., Holmlund, A., & Hellberg, D. (2015). Trends over 30 years in the prevalence and severity of alveolar bone loss and the influence of smoking and socio-economic factors — based on epidemiological surveys in Sweden 1983-2013. International Journal of Dental Hygiene 13(4), 283-91.
Ekstrand, K. R., & Qvist, V. (2015). The impact of a national caries strategy in Greenland after 4 years. International Journal of Paediatric Dentistry 25(4), 255-66.
Eurostat. (2006). Statistic Explained. File: Main indicators for health resources V2.png. Retrieved from: http://ec.europa.eu/eurostat/statistics-explained/index.php/File:Main_indicators_for_health_resources_V2.png
Fujita, M., Ueno, K., & Hata, A. (2009). Lower frequency of daily teeth brushing is related to high prevalence of cardiovascular risk factors. Experimental Biology and Medicine 234(4), 387-94.
Gerritsen, A. E., Allen, P. F., Witter, D. J., Bronkhorst, E. M., & Creugers, N. H. J. (2010). Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health and Quality of Life Outcomes 8, 126. doi: 10.1186/1477-7525-8-126.
Gorbatova, M. A., Gribovsky, A. M., Gorbatova, L. N., & Honkala, E. (2012). Dental caries experience among 12-year-old children in North-west Russia. Community Dental Health 29(1), 20-4.
Holm-Pedersen, P., Vigild, M., Nitschke, I., & Berkey, D. (2005). Dental care for aging populations in Denmark, Sweden, Norway, United Kingdom, and Germany. Journal of Dental Education 69(9), 987-97.
Honkala, E., Paronen, O., & Rimpela, M. (1983). Familial aggregation of dental health habits in Finland. Journal of Pedodontics 7(4), 276–90.
Honkala, E., Karvonen, S., Rimpelä, A., Rajala, M., Rimpelä, M., & Prättälä, R. (1991). Oral health promotion among Finnish adolescents between 1977 and 1989. Health Promotion International 6(1), 21-30.
Honkala, E., Kuusela, S., Rimpelä, A., Rimpelä, M., & Jokela, J. (1997). Dental services utilization between 1977 and 1995 by Finnish adolescents of different socioeconomic levels. Community Dentistry & Oral Epidemiology 25(6), 385-90.
Honkala, S., Honkala, E., Newton, T., & Rimpelä, A. (2011). Toothbrushing and smoking among adolescents – aggregation of health damaging behaviours. Journal of Clinical Periodontology 38(5), 442-8.
Johansson, V., Soderfeldt, B., & Axelius, B. (2007). Caries prevalence among children, adolescents and adults, and periodontal conditions among adults in Denmark, Finland, Norway and Sweden. Oral B’s Nordic Report on Oral Health. Malmö: Malmö University, Sweden.
Kassebaum, N. J., Smith, A. G. C., Bernabe, E., Fleming, T. D., Reynolds, A. E., Vos, T., Murray, C. J. L., Marcenes, W., & GBD 2015 Oral Health Collaborators. (2017). Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990-2015: A systematic analysis for the global burden of diseases, injuries, and risk factors. Journal of Dental Research 96(4), 380-7.
Kidd, E., & Fejerskov, O. (2016). Essentials of Dental Caries, 4th ed. New York: Oxford University Press. ISBN: 9780198738268.
Kobayashi, Y., Niu, K., Guan, L., Momma, H., Guo, H., Cui, Y., & Nagatomi, R. (2012). Oral health behavior and metabolic syndrome and its components in adults. Journal of Dental Research 91(5), 479-84.
Kuusela, S., Honkala, E., & Rimpelä, A. (1996). Toothbrushing frequency between the ages of 12 and 18 years – longitudinal prospective studies of Finnish adolescents. Community Dental Health 13(1), 34-9.
Listl, S., Galloway, J., Mossey, P. A., & Marcenes, W. (2015). Global Economic Impact of Dental Diseases. Journal of Dental Research 94(10), 1355-61.
Lowe, G., Woodward, M., Rumley, A., Morrison, C., Tunstall-Pedoe, H., & Stephen, K. (2003). Total tooth loss and prevalent cardiovascular disease in men and women: possible roles of citrus fruit consumption, vitamin C, and inflammatory and thrombotic variables. Journal of Clinical Epidemiology 56(7), 694-700.
Löe, H. (2000). Oral hygiene in the prevention of caries and periodontal disease. International Dental Journal 50(3), 129-39.
Malik, V. S., Popkin, B. M., Bray, G. A., Despres, J.-P., Willett, W.C., & Hu, F.B. (2010). Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes. Diabetes Care 33(1), 2477-83.
Malmö University. (2016). Oral Health Database. Country Oral Health Profiles. Retrieved from: https://www.mah.se/CAPP/Country-Oral-Health-Profiles/
Marcenes, W., Kassebaum, N. J., Bernabé, E., Flaxman, A., Naghavi, M., Lopez, A., & Murray, C.J. (2013). Global burden of oral conditions in 1990–2010: a systematic analysis. Journal of Dental Research 92(7), 592-7.
MMWR. (2011). Dental caries in rural Alaska Native children – Alaska, 2008. Morbidity and Mortality Weekly Report 60(37), 1275-80.
Moynihan, P., & Petersen, P.E. (2004). Diet, nutrition and the prevention of dental diseases. Public Health Nutrition 7(1A), 201-26.
Mueller, H.-P. (ed.) (2015). Periodontology – The Essentials, 2nd ed. Thieme Publishers Stuttgart. Print ISBN: 9783131383723. E-book ISBN: 9783131648723.
Okoro, C.A., Balluz, L. S., Eke, P. I., Ajani, U. A., Strine, T. W., Town, M., Mensah, G. A., &
Mokdad, A. H. (2005). Tooth loss and heart disease – Findings from the behavioural risk factor surveillance system. American Journal of Preventive Medicine 29(5 Suppl 1), 50-6.
OECD, Organisation for Economic Co-Operation and Development. (2016). Health Care Resources: Dentists. Retrieved from: http://stats.oecd.org/Index.aspx?DatasetCode=HEALTH_STAT
Perez, M., Sheiham, A., Liu, P., Demarco, F. F., Silva, A. E. R., Assunção, M. C., Menezes, M., Barros, F. C., & Peres, K. G. (2016). Sugar Consumption and Changes in Dental Caries from Childhood to Adolescence. Journal of Dental Research, 95(4), 388-94.
Petersen, P. E. (2003a). The World oral health report 2003: continuous improvement of oral health in the 21st century – the approach of the WHO Global Oral Health Programme. Community Dentistry & Oral Epidemiology 31(Suppl 1), 3-24.
Petersen, P. E. (2003b). Tobacco and oral health – the role of the World Health Organization. Oral Health & Preventive Dentistry 1(4), 309-15.
Petersen, P. E. (2009). Global policy for improvement of oral health in the 21st century – implications to oral health research of World Health Assembly 2007, World Health Organization. Community Dentistry & Oral Epidemiology 37(1), 1-8.
Raittio, E., Kiiskinen, U., Helminen, S., Aromaa, A., & Suominen, A. L. (2015). Income-related inequality and inequity in the use of dental services in Finland after a major subsidization reform. Community Dentistry & Oral Epidemiology 43(3), 240-54.
Rajala, M., Honkala, E., Rimpelä, M., & Lammi, S. (1980). Toothbrushing in relation to other health habits in Finland. Community Dentistry & Oral Epidemiology 8(8), 106-13.
RHIhub, Rural Health Information Hub (2002-2018). Rural Oral Health Toolkit. Retrieved from: https://www.ruralhealthinfo.org/community-health/oral-health
Rose, G. (2001). Sick individuals and sick populations. International Journal of Epidemiology 30(3), 427-32.
Schroth, R. J., Smith, P. J., Whalen, J. C., Lekic, C., & Moffatt, M. E. K. (2005). Prevalence of caries among pre-school-aged children in a northern Manitoba community. Journal of Canadian Dental Association 71, 27. Retrieved from: http://www.cda-adc.ca/jcda/vol-71/issue-1/27.pdf
Sheiham, A. (1970). Dental cleanliness and chronic periodontal disease. Studies on population in Britain. British Dental Journal 129(9), 413-8.
Sheiham, A. (1983). Sugars and dental decay. Lancet 1(8319), 282-4.
Sheiham, A., & Watt, R. G. (2000). The Common Risk-Factor Approach: a rational means of promoting oral health. Community Dentistry & Oral Epidemiology 28(6), 399-406.
Sheiham, A. (2001). Dietary effects on dental diseases. Public Health Nutrition 4(2B), 569-91.
Stoltenberg, J. L., Osborn, J. B., Pihlstrom, B. L., Herzberg, M. C., Aeppli, D. M., Wolff, L. F., & Fischer, G. E. (1993). Association between cigarette smoking, bacterial pathogens, and periodontal status. Journal of Periodontology 64(12), 1255-30.
Te Morenga, L., & Mann, J. (2012). The role of high-protein diets in body weight management and health. British Journal of Nutrition 108(Suppl 2), S130-8.
Vikum, E., Krokstad, S., Holst, D., & Westin, S. (2012). Socioeconomic inequalities in dental services utilization in a Norwegian county: The third Nord-Trøndelag Health Survey. Scandinavian Journal of Public Health 40(7), 648-55.
Virtanen, J. I., Berntsson, L. T., Lahelma, E., Kohler, L., & Murtomaa, H. (2007). Children’s use of dental services in the Nordic countries. Journal of Epidemiology & Community Health 61(12), 1080-5.
United Nations (UN). (2011). Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. Resolution A/66/L.1. New York: United Nations. Retrieved from: http://www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf
Walsh, T., Worthington, H. V., Glenny, A. M., Appelbe, P., Marinho, V. C., & Shi, X. (2010). Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents. Cochrane Database Systematic Reviews (1), CD007868. doi: 10.1002/14651858.CD007868.pub2.
WHO. (2000). Oral Health Programme. Global data on dental caries prevalence (DMFT) in children aged 12 years. Geneva: World Health Organization. Retrieved from: http://www.who.int/iris/handle/10665/66520
WHO. (2015). WHO report on the global tobacco epidemic, 2015. Raising taxes on tobacco. Geneva: World Health Organization. Retrieved from: http://apps.who.int/iris/bitstream/10665/178574/1/9789240694606_eng.pdf?ua=1&ua=1
Widström, E., Ekman, A., Aandahl, L. S., Pedersen, M. M., Augustsdottir, H., & Eaton, K. A. (2005). Developments in oral health policy in the Nordic countries since 1990. Oral Health & Preventive Dentistry 3(4), 225-35.
Widström, E., Koposova, N., Nordengen, R., Nergdahl, M., Eriksen, H., & Fabrikat, E. (2010). Oral health care and dental treatment needs in the Barents region. International Journal of Circumpolar Health 69(5), 486-99.
Zimmermann, H., Zimmermann, N., Hagenfeld, D., Veile, A., Kim, T. S., & Becher, H. (2015). Is frequency of tooth brushing a risk factor for periodontitis? A systematic review and meta-analysis. Community Dentistry & Oral Epidemiology 43(2), 116-27.