Education Theory Made Practical, Volume 4 by McMaster Program for Faculty Development is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.
Education Theory Made Practical, Volume 4 by McMaster Program for Faculty Development is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.
1
2
Funding
This work has been funded by a generous grant from eCampus Ontario, which is an initiative of the Government of Ontario (Canada).

Usage
Available for usage under the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.

Where can I find this online?
This book can be found in the ALiEM Library (aliem.com/library), Apple Bookstore, ResearchGate, and the Government of Ontario’s eCampus library.
Editors
Sara M. Krzyzaniak, MD
Anne Messman, MD
Daniel Robinson, MD, MHPE
Benjamin Schnapp, MD, MEd
Simao Li-Sauerwine, MD, MSCR
Michael Gottlieb, MD
Teresa Chan, MD, MHPE
Foreword
Jonathan Sherbino
3
My first course in grad school was “Theory in Higher Education.” I confess to being lost and slightly bewildered during the initial classes. It felt like the first months of medical school with a new language to master and new ways to organize knowledge. My solution to my confusion was to find the four other physicians in the class. (The other students were already well versed in this lexicon via their previous social science or humanities education.) Each Tuesday evening, after the class concluded at 10:00 PM, the five of us would meet at a local restaurant and try to decipher what happened. New words we attempted to define. More importantly, we tried to decipher the theories presented in class. (This predated Google and instantaneous access to resources such as Education Theory Made Practical [ETMP].) Over time I became less clumsy with the language, and I began to appreciate how a theory could organize, predict, expand, or challenge the concepts and ideas I was encountering as a very new clinician-educator.
For a time, I imagined that there was a meta-framework that connected, ordered, and ranked all education theories. In hindsight, I perceive the influences of my medical training and the hidden (or perhaps not so hidden) influence of evidence-based medicine with its associated hierarchy of evidence. As a new educator, I struggled to find the “right” theory to explain or understand a phenomenon. With time, experience, and great mentoring, I realized the problem with such an approach.
Medical education is not a discipline with discrete borders, specific methods and accepted theories, like molecular biology. Rather it is a field with fuzzy boundaries, informed by the sciences, social sciences and humanities and drawing upon their mix of associated theories.1 Neuroscience, sociology, and philosophy all have an equal place in medical education. Medical education is richer for such interconnectedness, requiring a negotiation and collaboration between different ways of seeing the issue confronting a clinician-educator. Deductive approaches to medical education research that use experimental data to support or refute a theory are complimented by inductive approaches, where theory is constructed from data without any presupposed starting position. In this way, medical education can use multiple theories to help make sense of the issues confronting learners, teachers and educators.2 But, unlike the clinical domain clinician-educators simultaneously reside in, there is no hierarchy of better/best theories in medical education. There is no one theory to rule them all. The issues in medical education are too nuanced and complex for such a rigid approach.
Here lies the value of ETMP. While I have specific theories (looking at you Cognitive Load Theory) that I draw on more regularly, I appreciate a vast number of theories relevant to my work in medical education. While I have grown as a clinician-educator since my first grad school course, there is still much for me to discover and learn. ETMP introduces to me, in an applied manner, theories that can bring fresh insight or better explanation to the questions I face in my education practice. Krzyzaniak, Messman, Robinson, Schnapp, Li-Sauerwine, Gottlieb, and Chan have edited a concise, well-referenced, practical, and highly readable resource for clinician-educators, regardless of level of experience. I look forward to discovering Joplin’s model of experiential learning, while contrasting it with the chapter on Kolb’s experiential learning. Scanning the table of contents reveals chapters relevant to teaching, learning, assessment, wellness, and more.
I wish I had ETMP when I started grad school. I prescribe it to my grad students and medical education fellows now. Volume Four is an excellent addition to the cannon of ETMP.
Jonathan Sherbino, MD, MEd
Professor of Medicine
Assistant Dean of Health Professions Education Research
McMaster University
4
This book is dedicated to all of the health professions educators who have been tirelessly improving education for their trainees throughout the global pandemic. We would like to thank Academic Life in Emergency Medicine for its continued support of the Faculty Incubator and medical educators in general – and in particular Dr. Michelle Lin for her continued leadership and sponsorship of our team.
Most importantly, we would like to thank the members of the 2019-2020 class of the ALiEM Faculty Incubator who have worked so diligently on creating this book, which will help other educators understand and apply educational theory. We hope you are proud of the scholarly work you have accomplished here, we surely are! We are also so proud of everything else you accomplished during 2019-2020 while balancing clinical responsibilities and all the additional burdens of pandemic life. We can’t wait to see what you all accomplish next.
Sara M. Krzyzaniak, MD
Anne Messman, MD
Daniel Robinson, MD, MHPE
Benjamin Schnapp, MD, MEd
Simao Li-Sauerwine, MD, MSCR
Michael Gottlieb, MD
Teresa Chan, MD, MHPE
1
Authors: Sonia Twigg, Andy Little, Moises Gallegos
Editor: Sara Krzyzaniak, MD
It’s a nightshift in your busy ED. The ED is pumping and Sarah, a senior resident, is running the pod. She has seen sick patient after sick patient and knows there are still long waits for patients in the waiting room. She is going as fast as she can and juggling as many patients as possible.
She is seeing Mr. Smith, her fifth patient with chest pain this shift. Mr Smith is in his 60s and has a typical presentation for ischemic chest pain: heavy central chest pressure for the past 30 minutes. He is hemodynamically stable and his pain improves after aspirin and sublingual nitro. His ECG shows ST depressions in V1-V3. Sarah makes sure she follows the department’s chest pain protocol including orders for serial troponins and ECGs, as well as sublingual nitro as needed. She expects Mr Smith has had a NSTEMI.
Another critical patient arrives, so she drops what she is doing to go and care for that patient. 30 minutes later she is called to Mr. Smith’s bedside by his nurse who is concerned that he is looking worse. Mr. Smith is diaphoretic, tachycardic, and has become hypotensive. Reviewing the initial ECG, her attending points out that the ST depressions in the anterior leads are concerning for a posterior STEMI. The attending orders a posterior lead ECG which demonstrates ST elevations in V7-V9, confirming her suspicion.
Sarah is upset about this missed diagnosis and the delay in care that it created. She wonders if she would have been able to arrive at the correct diagnosis if she had not been distracted by her other patients and frequent interruptions.
Cognitive Load Theory builds on Atkinson and Shiffrin’s model for human memory.3 Sensory inputs enter into our working memory, and we organize (“chunk”) this information into “schemas” that are then stored in long term memory. Working memory is limited. At any given time we can hold 7+/- 2 items in our working memory for only 30 seconds. Long term memory is infinite, but we have to retrieve the schemas back into working memory when we need them. Working memory becomes the bottleneck for learning. Over time, and with repeated experiences, specific schemas become more complex, organized and eventually automated — this is expertise.4 A single schema, however complex, counts as one item in working memory. The premise of CLT is that the processes of learning may be different from the processes required to complete a task. If working memory is spent on tasks that do not contribute to the development of schemas from working memory to long-term memory, learning cannot occur.
Intrinsic load describes the cognitive demand of the task itself.2 Intrinsic load is affected by task complexity and the prior knowledge of the learner. Complex tasks, with a high number of elements or highly interactive elements, impose a higher intrinsic load than simple tasks.3 Let’s use the example of analyzing an ECG. Rare or subtle ECG findings are harder to pick up than obvious ones. Novice learners experience a higher intrinsic load than experienced learners doing the same task. An experienced senior resident would be expected to analyze the same ECG faster and more accurately than a medical student.
Extraneous load is the extra information we experience that is not necessary to complete the task yet uses up part of our precious working memory.2 It’s what gets in the way of doing the task: the buzzer that goes off while you are reading the ECG, the interruption with a question, the poor print out, and the time pressure of the busy ED. Each of these work to increase your cognitive load and make reading the ECG harder. But it’s not always bad! Sometimes the extra information helps you elaborate the schema. For example a quick review of STEMI mimics from an online reference before reading the ECG may help you make the correct interpretation of the ECG.
Germane load describes the effort associated with learning. It is the load we experience from processing the information in our working memory into (or out of) the schemas we store in long term memory.3 It is closely linked with intrinsic load, but it relates more to the attention devoted to learning rather than the effort dedicated to actually performing the task (i.e. intrinsic load).
Overview
In a series of papers during the 1980s, Sweller1 began to outline his observations that a high cognitive load negatively impacts learning.
“Cognitive load” is composed of intrinsic load, extraneous load, and germane load.
Germane load can be thought of as the process of learning. If the intrinsic and extraneous load are too great, we become cognitively overloaded and have little to no capacity for germane load – we can’t learn!
Cognitive Load Theory (CLT) suggests we should design education and performance systems that2:
Man Originators of the Theory
John Sweller
Other important authors or works:
In 2010 Van Merrienboer and Sweller offered principles to guide instructional design in medical education.4 Fraser et al. elaborate on them in their 2015 review of how CLT applies to healthcare simulation.5
Strategies to manage intrinsic load:
Strategies to decrease extraneous load:
Strategies to optimize germane load:
Cognitive load & instructional design:
Leppink describes three dimensions that help guide instructional design6:
He recommends that fidelity and complexity should be gradually increased while ensuring adequate instructional support, and then ultimately fade the instructional support when it is no longer needed.
These principles help explain the “expertise-reversal effect”. As the learner becomes more advanced, techniques that previously augmented learning for the novice actually start to interfere. For example, asking an expert to use an unfamiliar mnemonic for a task they already do well provides too much instructional support which increases extraneous load.
A fundamental characteristic of health professions is the collaborative nature of care. Research has begun to explore the application of CLT to group-based learning and teamwork. Kirschner et al have promoted the “interaction hypothesis” to explain the differences in learning efficiency for groups and individuals.7,8 They discuss the impact of utilizing a combined, or collective, working-memory, in the development of schema. In a group setting, cognitive load can be distributed to the working memory of various team members for processing. Large quantities of information are serially distilled into workable inputs that team members can then use to form schema. This can be useful when dealing with high complexity tasks that would otherwise overload an individual. However, with low complexity tasks, distribution of cognitive load may leave individuals without enough effortful processing of information to allow for appropriate schema development. It becomes “a trade-off between the group’s advantage of dividing information processing amongst the collective working memories of the group members and its disadvantage in terms of associated costs of information communication and action coordination.”7
Fraser et al have begun to look at how emotion affects cognitive load.5 They point out that the activation of emotion is inevitable in healthcare simulation, among other situations in medicine. Emotion can increase extraneous load, but it is sometimes an important component of intrinsic load, e.g. when learning to break bad news. Positive emotions appear to improve learning, perhaps through improving motivation and attention or through improving problem solving and creativity. Stress appears to have varying effects; it can focus attention and improve schema formation for the task at hand, but it also decreases working memory and can impair retrieval from long term memory. Healthcare teams have been shown to increase performance when feeling psychologically safe, so if psychological safety is present, “academic emotions,” such as performance anxiety and motivation to learn, can be optimized.
The argument can be made that the Flipped Classroom model for teaching benefits from application of CLT by creating protected learning time through removing it both temporally and spatially from preparatory time.9 The inherent separation of preparatory work from active application creates a focus on germane load during in-person sessions and off-loads intrinsic and extraneous processes. The design principles proposed by Van Merrienboer and Sweller to improve the balance of cognitive load in health professions education can be applied to optimize the preparatory material and in-person sessions that create a flipped learning experience.4
Simulation-based learning forms an important tenet of skill development and critical action decision making. However the complexity of cases and skills taught through simulation may result in too high a cognitive load. CLT can be applied to simulation curricula for improved results.5 While running a simulated pediatric resuscitation, a trainee may become overwhelmed trying to remember medication dosages and lose track of the experiential goals for the session. Providing a Broselow tape, or better yet a confederate such as a pharmacist, would allow the learner to focus on building skills as a team leader.
CLT has been applied to performance in medicine as well as learning. Sewell examined cognitive load as it applies to performing a colonoscopy.10 The same group has also looked at how cognitive load impacts patient handovers.
De Jong criticized CLT by pointing out that while it describes a cognitive basis for instructional design principles, it is “impossible to falsify” because CLT relies on post-hoc assumptions.12 If the load imposed by the task interferes with our schema construction, we think it’s bad and label it as extraneous load. If it helps us construct schema, then we think it’s good and label it as germane load. In other words, we make the evidence fit the theory.
Perhaps we could justify this labeling if we could directly or accurately measure cognitive load. Current measures include:
Psychometric testing. Paas developed and validated a single-item scale, which is the most commonly used measure.13 In contrast the NASA-Task Load Index (NASA-TLX) is a multi-item scale.14 Unfortunately these are self reported measures that occur after the task has finished. They may not reflect the load during the task, and they only measure overall cognitive load.
Secondary task response. The speed and accuracy of performing a secondary task, for example giving a medication order while reading the ECG. While you are concentrating on that complex ECG, you might start mumbling or pausing while giving the medication order.
Physiologic measures. Heart rate or respiratory rate variability, EEG or EMG monitoring, eye tracking, pupillary diameter, blink frequency, serum adrenaline levels, brain imaging and skin conductance have all been examined and validated. Their supposed advantage is that they can measure cognitive load instantaneously and continuously over time.
Performance on the task.3 Examining how well is the task performed, e.g. number of errors made during task, can provide insight into how much cognitive load was involved in the performance.
It is arguable whether these are valid or accurate measures. What are they really measuring? While they are general measures of cognitive load, most do not measure its constituent parts of intrinsic, extraneous and germane load. In other words, they can tell us that cognitive load affects performance but not how the different parts interact.
In 2013, Leppink developed a psychometric instrument to differentiate between different types of cognitive load.15 However in a subsequent review, it was noted that some studies did not support the instrument described.6 The authors of the review suggested that we go back to a two factor framework and think of cognitive load as consisting of only intrinsic and extraneous load along with a “subjective judgement of learning.” Young and Sewell disagree and have derived instruments to measure the different types of load in medical settings including colonoscopy10 and patient handovers.16 In 2016, Naismith developed the Cognitive Load Component (CLC) psychometric test and compared it with the Paas and NASA TLX tests.17 This interesting but small study showed little agreement on total cognitive load between the three tests. However intrinsic load seemed consistently measured by all three. Intrinsic load on the CLC correlated with the NASA TLX subscales of mental demand and frustration.
CLT makes intuitive sense, but we have more research to do to demonstrate how it applies to instructional design and workplace performance.
After her whirlwind shift, Sarah is finally able to catch her breath and reflect on Mr. Smith’s case. Luckily he was taken to the cath lab 20 minutes after discovering the posterior MI where emergent PCI and stenting of a 90% occluded RCA occurred without complications and he was transferred to the CCU in stable condition.
She recognizes that as a senior resident she should be more capable of identifying this common ECG pattern. She plans to spend some time on her day off studying ECGs (decrease intrinsic load) and will set a systematic approach for when she is handed ECGs on shift making sure she pauses for each (decrease extraneous load).
Annotated Bibliography
1. Van Merrienboer JJ and Sweller J. Cognitive load theory in health professions education: design principles and strategies. Med Educ. 2010;44: 85-93.
This paper gives the clearest advice on pragmatic strategies for incorporating CLT into the design of medical education curriculum of all types.
2. Young JQ, Van Merrienboer J, Durning S et al. Cognitive load theory: implications for medical education: AMEE Guide No. 86. Medical Teacher. 2014;36:371-384.
This guide clearly describes CLT in terms of its origins in models of human memory, its relation to other learning theories, and how expertise is developed.
3. Sewell JL, Maggio L, ten Cate O et al. Cognitive load theory for training health professionals in the workplace: A BEME review of studies among diverse profession: BEME guide No. 53. Medical Teacher. 2019;41(3):256-270.
Sewell et al provide a scoping review of CLT literature. Specifically they discuss practice points for workplace teaching, curricular design, learning environment, and metacognition. They conclude that CLT alone cannot account for the complex environment created by health profession education workplaces and would benefit from integration with other education theories and frameworks.
4. Kirschner PA, Sweller J, Kirschner F, Zambrano R J. From cognitive load theory to collaborative cognitive load theory. Int J Comp Supported Collab Learn. 2018;13(2):213-233.
This paper provides a review of the principles in human cognitive architecture that first led to CLT, how CLT can be applied to instructional design, and how CLT can be combined with the cognitive interdependence principle to create Collaborative Cognitive Load Theory.
2
Authors: Krystin Miller, MD; Kelsey Vargas, MD; Guy Carmelli, MD
Editor: Simiao Li-Sauerwine, MD, MSCR
John, a senior resident in emergency medicine, just opened the chart of Mr. Smith on a busy Monday afternoon shift. He thought the name sounded familiar, and in fact he had seen the patient before. The patient has visited the emergency department several times for chronic back pain, most recently one week ago. Prior clinicians have documented concern for drug-seeking behavior. Begrudgingly, John prepares to go see the patient. Today, the patient’s chief complaint is back pain and leg pain.
John takes a very abbreviated history from the patient. John feels like this is a difficult patient encounter, as the patient is grumpy and uncooperative and is asking repeatedly for pain meds. Mr. Smith answers simple yes or no questions but fails to provide additional details. However, John doesn’t push back with any follow-up questions. At the same time as he is interviewing Mr. Smith, John is filling out his chart and also interrupting the patient several times to ask a nearby nurse about his other patients.
John determines Mr. Smith is having low back pain that is radiating to his feet. The patient was witnessed during examination to have an antalgic gait. Mr. Smith has no “red flag symptoms” including trauma, malignancy, incontinence to bowel or bladder or new neurologic deficits. The patient was examined fully dressed, but John feels he has obtained an adequate exam for the complaint. John determines there is no indication for further testing or imaging at this time. John communicates with the attending that the patient’s pain is likely an exacerbation of his underlying degenerative disc disease and sciatica. He would like to offer the patient acetaminophen for pain and discharge to home without further diagnostics.
Prior to the attending seeing the patient, the patient’s nurse approaches the team and states, “I’ve taken care of Mr. Smith before, and he just doesn’t seem himself. His vitals today are abnormal. He has a slight fever with tachycardia and his blood pressure is lower than he usually runs. I am concerned we might be missing something here.”
The attending sends John back to the bedside to re-evaluate the patient.
Ronald Epstein is the founder of mindfulness in medicine. Ronald Epstein matured in an age of counterculture and the partnered threats of conflict in the mid-20th century. This era of turmoil led to a life-long practice that has become integral in his daily practice.4 Epstein’s father served as an army physician and Epstein himself went through the motions of what was expected: attending university with the expectations of becoming a doctor. However, while he was finishing up college, he felt that something was missing. Early 20th-century medicine had evolved into viewing the human body as a machine, and the mechanics (i.e. doctors) fixed machines. This practice was at odds with how Epstein viewed the overall goals of medicine. In 1971, he took a course in Transcendental meditation and this gave him a glimmer of light. He eventually left school and moved to the West Coast where his journey through meditation began.
His route back to medicine was to discover research on the medical benefits of meditation, eventually choosing Harvard Medical School, a powerhouse of innovative research. His research unearthed studies suggesting that blood pressure, chronic pain, anxiety, and other medical conditions could benefit from meditation. He graduated medical school and became a family medicine practitioner who incorporates traditional holistic teachings into patient care. He turned meditation into mindfulness in practice– incorporating the fundamentals of meditation into clinical shifts and the struggles that physicians face day-to-day.2
The foundation of Zen Buddhism cultivates present moment-to-moment awareness and awareness of self. It begins with a quiet setting, relaxing in a comfortable position, and focusing on breathing. When the mind starts to wander, it purposefully brings itself back to the focus on each individual breath. Each wander becomes shorter until the mind is clear enough to be in the present moment alone. Mindfulness is attending to the ordinary, the obvious, and the present.2 To see the ordinary in a day full of critically ill patients is to see the family member that continues to ask for updates because they are scared and confused and to understand that your frustration is not with this family member, but with the workload, the lack of resources, and the inability to save each patient.
A second purpose of Zen is awareness of self— to understand one’s own thoughts, feelings, and flaws.4 Zen is the ability to allow the emergence of feelings without attempting to change or judge them, permitting these feelings to “just be.” However, a second foundation is living selflessly, understanding that there are times when a feeling does require change. One of Epstein’s stated goals was to “have more intentional unselfish awareness moments than selfish ones.” It is considered a universal human capacity to foster clear thinking and open-heartedness.1
Applying this process to patient care requires the provider to actively observe the patient, themselves, and themselves with the patient. Physicians are human, therefore one should attempt to understand inherent biases that are brought to a patient encounter in order to empathize and connect with the patient for improved care.
Overview
Mindfulness is a derivation of Zen Buddhist meditation. The general teaching is on being focused on the present and maintaining moment by moment awareness.1 Mindfulness has since transitioned into the medical field, beginning in medical school curricula, encouraging budding students to listen more attentively to their patients, become more aware of their own mental processes, and recognize their own biases and judgements.2 Mindfulness practices have been shown to better allow physicians to care for the patients through compassion and understanding.
In Emergency Medicine (EM), qualities deemed important to being a good EM physician include compartmentalizing, multi-tasking, and pattern recognition. However, while these traits generally allow EM physicians to more efficiently triage critical versus non-critical patients, these qualities may interfere with the holistic approach to treating the patient. The constant interruptions, patient overcrowding, inpatient boarding, and hospital oversight and policies all contribute to disengagement and reflexive thinking in many physicians’ decision-making processes.3
In contrast, mindfulness is a state of welcoming uncertainty in place of avoidance which frees up the physician from being limited by factors out of their control. Mindful practice opens up the physician to be aware of the complexity of the situation and his or her inherent biases in order to stop, think, and configure a treatment plan that encompasses what is best for the patient.
Main Originators of the Theory
Ronald M. Epstein
Other important authors or works:
Outcome based medical education echos constructive alignment theory, by orienting training on intended learning outcomes. As described by Biggs and Tang (2011), in outcomes-based teaching the question changes from which topics are taught to “What do I want my students to be able to do” after curriculum completion2. Medical schools have begun implementing such learning activities as problem based learning sessions, portfolio education exercises, and narrative exercises into undergraduate medical education. Medical simulation has become increasingly integrated into medical education at both undergraduate, graduate, and post-graduate continuing education levels and can serve as both a learning activity with team based learning or for assessment such as OSCEs for undergraduate medical education.
In more recent times of crises during the COVID-19 pandemic a need surged for education on management practices and personal protective practices across the world. Institutions have used this same framework to first identify the learning outcomes of safe care for potential COVID-19 patients, developed quickly implemented learning activities through teleconferences, discussions, and simulations to align for assessment of these critical skills. Assessment in some settings includes auditing by Infection Protection and Control (IPAC) experts.
Historically a Buddhist practice, mindfulness itself requires no religious or cultural affiliation, and rather can be used in any setting as our innate ability to foster clear thinking and open heartedness.1 The underlying philosophy of mindfulness is based on the interdependence of action, cognition, memory and emotion.1 Being that medicine is an intersection between art and science, mindfulness practices made an easy transition into the field of medicine.
The current era of medicine is filled with constant distractions, whether by email, cell phones, or other technological devices. The new age of medicine comes with increased demands to improve productivity often at the expense of the patient-physician relationship. Many physicians state that they lack sufficient time with patients to explore the depth of their experiences and how it relates to their medical presentation.3 Rather, pressure from administration and the medical system leads many practitioners to rely on instincts and first impressions to make quick decisions.
Mindfulness, a practice of nonjudgmental moment-to-moment awareness, is one way for physicians to become aware of these patterns of behavior, habits, and reactions.3 Patient-centered care emphasizes understanding the patient as a person and encouraging a more participatory patient-physician relationship.5 This type of relationship has the appearance of increased time requirements in a world where practitioners are suffering through multi-tasking and quick paces. However, one can make a meaningful connection by sitting down, engaging with the patient, and not rushing through depersonalized conversations. One uninterrupted encounter with the patient answering questions and explaining diagnoses and plans generally takes less time that multiple short, interrupted interactions where neither the patient nor the practitioner feel satisfied with the outcome.
Modern medicine makes room for different applications of mindfulness to suit the individual’s needs. Practitioners may keep a journal, meditate, or even review recordings of patient encounters.2 In medical education, learner self-evaluation forms are a great way for the student or resident to reflect on their experience and compare perceptions with their teachers and/or mentors.2 Furthermore, peer evaluations and critical incident reports can bring awareness to aspects of professionalism, difficult situations, gaps in medical knowledge and social skills for students, residents, and practicing physicians.2
Studies have been published showing the many positive benefits of practicing mindfulness. One publication showed that introducing a mindfulness-based stress reduction educational intervention to medical students led to a decrease in total mood disturbance.6 Another study showed that mindfulness training in students can reduce psychological distress and feelings of burnout, improve well-being and mood, and increase patient empathy.7,8 Finally, a qualitative study of primary physicians who received a mindfulness communication program showed that the physicians consequently felt a reduction in professional isolation, improvement in attentiveness, and an increase self awareness.9
Habits of mind, including use of attentiveness, curiosity, flexibility and presence, are important features for patient care and physician well being. Epstein discussed his 8-fold approach for teaching mindful practice in medicine:10
1) Priming- Setting the expectation of student self-observation.
2) Availability- Creating a quiet, uninterrupted space to interact.
3) Asking reflective questions– Questions designed to foster curiosity.
4) Active engagement– Being physically and mentally present with the student.
5) Modeling- Showing actions while “thinking aloud” to make the tacit explicit.
6) Practice- Disciplined repetition in controlled settings.
7) Praxis- Motivating students to put knowledge into practice.
8) Assessment and confirmation– Evaluate mindfulness and presence.
Evidence-based decision models are benefited by mindful practice– applying data from groups of patients to the care of one patient.5 However, this practice is limited by incomplete tacit patient information.2 Mindfulness can bridge the gap between evidence-based and relationship-centered care, overcoming the limitations of both approaches. Mindfulness helps a provider formulate a clinical question, find appropriate sources and then bring the information back to the bedside.
There are many examples of mindfulness practices in the hospital. One example is the “sterile cockpit rule.”11 In air travel, this rule prohibits any flight crew member from engaging in any non-flight related activity or conversation during a critical phase of flight. Similarly, this can be used in the operating room, during resuscitations, or prior to procedures. This mindfulness practice of being in the moment and free from distractions is an excellent clinical tool and application of the theory.
On re-evaluation, John confirms the patient is indeed febrile, tachycardic and now hypotensive. John decides to take a much more detailed history and perform a more thorough examination of Mr. Smith after he is completely changed into a hospital gown. John discovers that the patient has been sleeping in a homeless camp for the past month and has been out of his diabetes and hypertension medications for approximately 6 months. Over the last 3-4 weeks, the patient has developed wounds on both of his feet, which he was initially embarrassed to tell anyone about. He has been feeling progressively worse, with fever and chills for about one week now. Ultimately, the patient gets admitted to the hospital for sepsis and requires podiatric intervention.
John and the attending debrief about the patient encounter, and the attending asks John some reflective questions.
“What assumptions did you make when you first opened the chart?”
“What did you miss in that first interview with the patient?”
John reflects on the assumptions he made about the patient and his personal biases that he brought to the encounter – multiple ED visits, chronic pain, non-specific complaints, prior clinicians report of drug seeking behavior. He also stated that he rushed through the interview and wasn’t attentive to the patient’s non-verbal cues during the interview. While the patient was a difficult historian, John reflects that he did not ask appropriate prompting questions to build rapport and gain the patient’s trust.
“What changed the second time you went into the room, John?”
John mentioned that he was more actively engaged and brought a new mindset to the encounter. He started from square one, with a blank slate, ignoring previous documentation that could lead to the formation of biases. During the second encounter, John also worked to leave his personal judgements and opinions at the door, and be more present and in the moment during the interaction.
John and the attending concluded with a discussion on mindful practice with an emphasis on being aware of our own judgements and categorizations during clinical encounters. Mindful practitioners are able to put these aside to demonstrate compassion, treat the patient as a whole person, and be attentive to the patient’s needs.
Annotated Bibliography
1. Epstein RM. Mindful practice in action (II): Cultivating habits of mind. Families Systtems & Health. 2003;21:11-17.
This second article in a two-part series outlines Epstein’s eight-fold method for promoting mindfulness in medical education. The eight areas include; priming, availability, asking reflective questions, active engagement, modeling while thinking out loud, practice, praxis, and assessment and confirmation. For each of these areas, the article provides practical application of the theory to medical education.
2. Epstein RM. Just being. West J Med. 2001;174:63-65.
This article by Epstein, discusses the importance of self care, meditation, and mindfulness. It concludes with providing resources that offer instruction on the topic area, as well as strategies for health professionals to enhance their well-being.
3. Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008;300:1350-1352.
This JAMA commentary, published in 2008, provides a concise overview of the applications of Epstein’s theory of mindfulness in medicine. In this article, the authors consider mechanisms of mindfulness as well as clinical applications, and also discuss some limitations of the current research in the field.
3
Authors: Mark Keuchel, D.O.,Al’ai Alvarez, M.D.,Curtis Knight, M.D.
Editor: Teresa Chan, MD, MHPE
The interns had an upcoming simulation module on placing central lines. A small group of them decided to show up early to play around with the equipment and see if they can practice on their own. Each of them had either seen one performed or got to place one during medical school. Everyone had an idea of what the correct steps were and each one felt comfortable practicing without the assistance of an instructor giving them direct feedback.
John, one of the interns, grabbed the syringe and attempted to cannulate the internal jugular in the mannequin. He kept poking the neck and was getting frustrated. Jill, recalling some steps from when she did placed a line, took over. She started telling John her version of how it should be done. Jim read out loud the steps emailed for their asynchronous learning as Jill continued to attempt with the cannulation. Everyone was feeling frustrated without the teacher.
Overview
Dr. Laura Joplin’s theory suggests that all learning is experiential. According to Joplin’s theory, a person learns from “experiencing” and interacting with the subject. Dr. Joplin felt that experiential learning programs had two main responsibilities to the learner:
These two phases of learning are joined in the “action-reflection” cycle. According to Joplin, the simple provision of an experience by itself is not sufficient for learning; a learner’s reflection on the action is of critical importance.
The five-stage model describes an experiential learning strategy that combines the following stages: 1) Focus; 2) Action; 3) Support; 4) Feedback; 5) Debrief.
Feedback and support are critical throughout the process from the moment of initial action through the conclusion of the learning experience. This framework gives educators a model to deliberately strengthen the experiential nature of their course design, highlighting that it is the educator’s responsibility to provide a learner-centered education.
Main Originators of the Theory
Laura Joplin
Joplin’s five-stage model was created to be intentionally simple and define the act of learning, but is not a learning theory itself. The model is organized around a ‘hurricane-like cycle’ in which a challenging action occurs between the initial focus stage and the final debriefing. These ‘action-reflection’ cycles are differentiated from experience alone by incorporating a reflection process. The application of the cycles can be in either a ‘maxi’ or ‘mini’ scope, depending on the intent of the project; the cycle can focus on large-scale course design or a brief teaching moment or insight.
The first aspect of the model is the focus stage. It is here that the educator identifies the task and the attention of the learner becomes engaged. The educator is tasked to shine light on a specific topic to help orient the learner. The education must also be cautious not to be too specific, as this cause learners to have tunnel-vision. The focus stage is necessary to align the learner’s attention with the educator’s goals. Actions in the focus stage depend on the type of activity to be performed. A focus stage may be as simple as verbally discussing the goals or it may be more complex, such as reviewing an article before an action.
The second part of the model is the action stage. This stage of the model surrounds the learner in direct confrontation with an often-unfamiliar situation requiring the learner to engage in problem solving. The inherent stress of the situation gives the learner an “experiential” learning. Active learning is facilitated by participation rather than passively reading or watching a video. The learner must be given “responsibility” in the learning process, a component that is absent in textbooks where the author decides the sources. The education is responsible for ensuring the learning difficulty is appropriate for the learner. By actively engaging the learner, the brain is considered “on” and the new information can be processed and retained.
Modern takes on this Theory
The intentional aspect of Joplin’s five-stage model of experiential learning requires time and work that may not always be feasible in the clinical setting. Moreover, there is a generational difference in perception of teaching and learning. Because Joplin’s model can be applied in a “maxi” and “mini” scope, it is easily translatable in a busy shift. Knowing the five stages is important, and deliberate signposting of these steps may help learners better appreciate the process. Here’s how:
In a “maxi” application of Joplin’s model, consider the process of training as a team for a SimWars competition. A group of residents are selected to represent the department. Each one has a specific skill set needed for success, yet team cohesion is a very important characteristic of a winning team. A deliberate focus on developing this sense of teaming is a must. As the team practices different approaches to crisis resource management, the team must reflect on the efficiency and effectiveness of their communication styles. This aspect of teaming must be intentionally and consistently supported. The feedback must also be specific regarding the delegation of roles, the use of closed-loop communication, and the appropriate tone and delivery of orders. For every iteration, each of these areas must be addressed for improvement, including highlighting successfully performed tasks. Ultimately, the five stages are repeated using multiple sources of feedback; support and challenging occur as the team advances. Once ready, the team will demonstrate a well-rehearsed, cohesive implementation of crisis management. A final debrief is critical in order to further emphasize areas for improvement and celebrate successes.
Another example for the use of Joplin’s five stages is the framework for a residents-as-teachers model. By clearly defining the steps in successful learner-centered teaching, a junior teacher (residents) are able to be deliberate in their approach to teaching. Not only will they gain experience in mastery of the topics they are teaching, they will also apply the metacognition of effective teaching styles.
Joplin’s five-stage model is clear, deliberate and learner-centered – but teacher intensive. The time requirement and effort required for preparing adequate experiences and creating the feedback and debriefing to match the initial experience is not to be taken lightly. In order to be effective, Joplin’s five-stage model requires time and intentionality. On shift teaching using Joplin’s model may not be feasible as we often cannot put a patient through several iterations of a procedure. From a learner’s perspective, learning in this model can be exhausting, thereby defeating the point of a learner-centered teaching. It is important to cultivate buy-in from the learner and acknowledge early on that rapid cycles of observation and feedback may lead to feedback fatigue. Frequent check-ins are important, and the teacher must create a supportive learning climate for the learner to work independently with fewer intrusions.
The group of interns realized that experience alone is not effective to learn how to place central venous catheters. They needed an instructor to tell them what they were doing right and what they were doing wrong. When the teacher arrived, she used Joplin’s five-stage model to provide a deliberate method for reflection at each step of the cycle. This encouraged them to develop mastery at each step of the process. The key is not to simply be lucky with cannulating the vein. An experienced teacher can help guide the process and solidify technical skills for each step. The teacher offered individualized support for each learner. She gave specific feedback in the moment along with appropriate corrective actions. The teacher provided support for successful completion of each task. At the end of the workshop, each of the learner felt confident about their skills and was able to demonstrate mastery of the procedure. A debriefing session followed to discuss scenarios and offer troubleshooting tips. Simulation workshops are a great way to teach procedural skills, especially using Joplin’s five-stage model of experiential learning.
Annotated Bibliography
1. Joplin L. On Defining Experiential Education. Journal of Experiential Education. 1981;4(1):17-20.
This paper introduces the idea of the 5-stage model of experiential learning. Her model is organized around a “hurricane-like cycle” emphasizing a challenging action that occurs between an initial stage of focus and a final debriefing stage. Feedback and support are present throughout all stages.
2. Kolb DA. Experiential learning: Experience as the source of learning and development. Upper Saddle River, NJ: Prentice Hall; 1984.
This book by Kolb built upon earlier work and lead him to believe that knowledge acquisition was obtained through “transformation of experience.” His theory had 4 stages in a cyclical pattern: concrete experience, reflective observation, abstract conceptualization, and active experimentation. This is an interesting theory that overlaps and augments the work of Joplin and is worth comparing and contrasting.
4
Authors: Anita Thomas, MD, MPH, Brian Barbas, MD
Editor: Benjamin Schnapp, MD, MEd
It is a busy Sunday evening in your emergency department. Jared, a fourth year medical student, is completing his case presentation to Dr. Jones: “…so, in assessment, Sarah is a 2-year-old female with a 2 cm linear forehead laceration, that I think requires suture repair.”
“Sounds good,” Dr. Jones replies. Since she has never worked with Jared before, she asks, “Do you feel comfortable suturing?”
“Definitely, I’ve sutured a bunch on other rotations,” Jared replies.
Dr. Jones nods. She has two other learners to check in on and patients are piling up in the waiting room. She decides to trust Jared’s self assessment. “Okay, I’ll order the topical anesthetic, intranasal midazolam, and have the nurse administer the midazolam about 5 minutes before we go in.”
Dr. Jones then sees several other patients and realizes that it has been about 45 minutes since topical anesthetic was applied to Sarah’s laceration. She walks into the patient’s room just as the nurse is administering intranasal midazolam and Jared is setting up the laceration tray. After restraining Sarah and attempting to distract her with her parents’ phones, it becomes apparent that Sarah was not sedated sufficiently, resulting in her screaming throughout the procedure. Her parents are very distressed, intermittently in tears and angry with the whole healthcare team.
“He told us that she would be completely asleep!” Sarah’s parents exclaim, pointing at Jared.
Dr. Jones attempts to de-escalate the situation by highlighting the amnestic effects of midazolam and remarks that Sarah likely does not like being restrained. She reiterates that this is a common anxiolytic in this age group for this procedure and that she does not typically recommend full sedation for this type of procedure.
While Dr. Jones is talking to Sarah’s parents, Jared starts to irrigate Sarah’s laceration, causing Sarah to cry even louder. At this point, Dr. Jones says, “I think it might be better if I did the repair.”
Jared is confused, but he pushes the laceration tray towards Dr. Jones. He watches the rest of the procedure silently, annoyed and feeling out of place.
After the laceration repair, Dr. Jones rushes out of the room to see another patient. Jared lingers with Sarah and her parents, discussing post laceration repair care. After several minutes, he steps out of the room to grab a popsicle for Sarah. He plans to discuss what happened, but by the time he had a moment to grab Dr. Jones, she had left for the day. Both of them were left wondering how the situation could have gone better.
Overview
As the name suggests, Kolb’s theory of experiential learning posits that much of learning takes place as we make sense of the experiences that we have. The four steps of Kolb’s theory are: concrete experience, reflective observation, abstract conceptualization, and active experimentation. Learning processes that are directly across from each other on the learning cycle (Figure 1) are related. Concrete experience and abstract conceptualization can be viewed as grasping experiences whereas reflective observation and active experimentation as transforming experiences.1
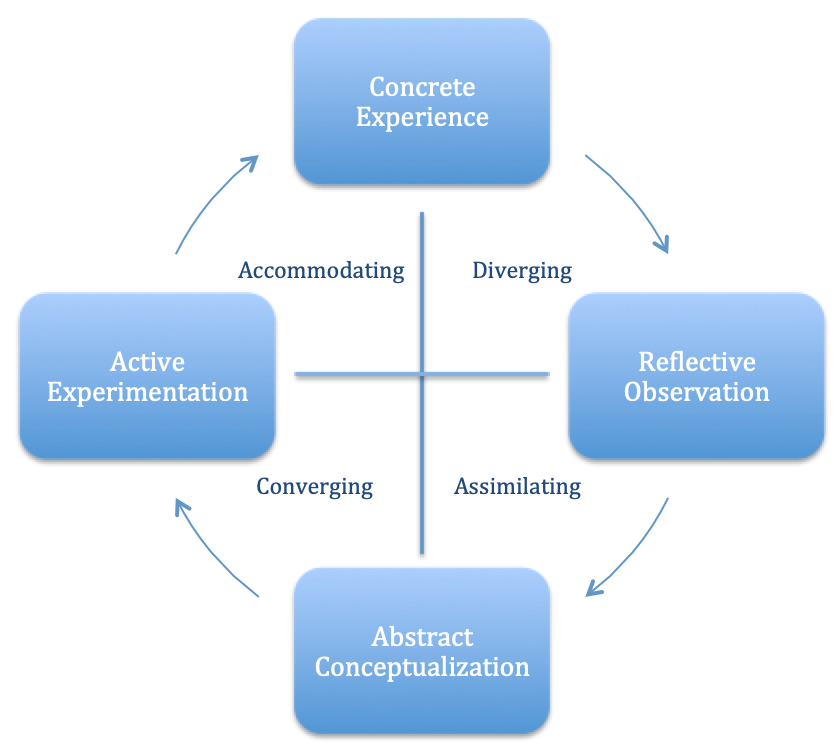
Figure 1: A graphical depiction of Kolb’s learning cycle, with the arrows indicating the traditional order of each step.2
Main Originators of the Theory
David Kolb
While first published in 1984 by educational theorist David A. Kolb, the influences behind experiential learning theory (ELT) can be found in the works of many before him including John Dewey, Kurt Lewin, Jean Piaget, and many more.
The concept of experiential learning can be seen as far back as the teachings of Confucious around 450 BC: “Tell me, and I will forget. Show me, and I may remember. Involve me, and I will understand.”3 In the early 20th century, this concept took hold in modern educational theory. During this time period, psychologist John Dewey posited that “there is an intimate and necessary relation between the process of actual experience and education.”4
During the 1940s, while studying group dynamics, social psychologist Kurt Lewin and his colleagues made note of the experiential learning process at work. While exploring the conversation about “the differences of interpretation and observation of the events by those who participated in them,” Lewin observed that learning is best facilitated in a setting in which there is an active balance between immediate concrete experiences of learners and the detached analytic feedback of the group.1 This lead to the creation of the National Training Laboratory in Group Development, which inspired the learning cycle at the base of Kolb’s ELT.1
Meanwhile, Piaget’s work exploring the cognitive-development process in childhood led to the development of another learning theory. Through his studies, Piaget argued that “intelligence arises as a product of the interactions between the person and his or her environment.”1 In other words, as Kolb summarized Piaget’s work, “intelligence is shaped by experience.”1
Experiential learning is essential to all of medical education. Nearly all of residency is an experiential learning process involving concrete experience, reflective observation, abstract conceptualization, and active experimentation under supervision. Kolb’s theory is so ingrained within medical education that most literature on practical application of Kolb’s ELT is related to clinical applications. Every patient interaction, new procedure, and bedside teaching moment with a medical student is an opportunity to witness Kolb’s ELT in action. Multiple times in a shift, a residents has a concrete experience, reflects on the experience, thinks of a plan to improve, and applies the changes on the next similar experience. In studies of resident education, Kolb’s ELT serves as at least a partial explanation for what is retained, highlighting the importance of trainees’ patient encounters.5,6
Clinically: Kolb’s theory of experiential learning can be applied to almost any patient encounter, but clinicians (including medical students, residents, and fellows) must actively engage in the steps. Reflection may be more likely after recognized medical errors, but the goal is for it to occur after almost every patient encounter. For example, a trainee might attempt to reduce a pediatric nursemaid’s elbow, which was actually been a supracondylar fracture. Discovering this on x-ray may lead to reflection and abstract conceptualization of why this patient had a fracture rather than a nursemaid’s elbow. Active experimentation would occur as they create their treatment plan for their next pediatric patient with elbow pain.
Classroom: Kolb’s theory applies well to the simulation environment. Simulated patient scenarios provide a concrete experience. Debriefing encompasses reflective observation and abstract conceptualization. Debriefings often start with open-ended questions such as “How did that feel?” allowing for the group to begin the process of reflective observation while discussing the most salient points of the case. Reviewing and reflecting on that shared experience ideally results in abstract conceptualization. For instance, a facilitator may start a discussion with, “Tell me about how you were thinking about whether to give fluids for this patient,” which can lead to a shared mental model of why fluids were desired and in what quantity. Active experimentation, or trying out variations on what was learned, can then be accomplished in subsequent simulations and in real patient encounters. Simulation can allow for all four steps of Kolb’s theory in quick succession by stopping participants when an error is made, offering immediate time for reflection and learning (which is not generally present in the real clinical environment), and repeating the simulation from the beginning so that active experimentation with new knowledge can be put into practice right away, a technique called rapid cycle debrief practice.9
Additionally, Kolb’s theory can be applied to morbidity and mortality (M&M) conferences, which start with a concrete clinical experience that has an unanticipated outcome, then allows for reflective observation and abstract conceptualization about more ideal management with the group. For example, if a patient with a headache after a concussion was ultimately diagnosed with a brain tumor after several clinical visits, the case serves as a surrogate concrete clinical experience for the primary clinician. Specifics of each visit, including the history, exam, and decision making, are generally reviewed during the conference, thus creating a shared mental model for all attendees. Generally, groups then reflect on each visit and discuss the clinical scenario. Often, other clinicians will utilize abstract conceptualization with comments like “Well, if I had been the primary doctor, then I may have ordered head imagine because of multiple visits,” or “I probably would have treated the patient similarly because of lack of concerning symptoms.” The purpose of M&M conferences is to reflect and increase awareness of such cases, such that attendees keep them in mind and potentially change their behavior when seeing similar patients in the future — a perfect example of active experimentation.
Kolb can be utilized as a framework for workshops as well. Structuring workshops with breakout sessions allows participants to reflect on their concrete experience. It also provides time to apply concepts learned during the workshop and conceptualize ways to change/improve their practice. Depending on the workshop topic, a workshop may allow for active experimentation as well. For example, in a quality improvement workshop, participate could be asked to reflect on quality issues the have experienced (concrete experience), think about how they have been addressed (reflective observation), consider what makes for a successful quality improvement project (abstract conceptualization), and brainstorm an opportunity for improvement in their own clinical environment (active experimentation).
It can be difficult to accomplish all of Kolb’s stages in a real clinical environment as it requires deliberate reflection and repeated experiences. In an emergent situation, like performing CPR on a dying patient, there might not be time to guide a learner through reflection, conceptualization, and experimentation. Additionally, the goal for a learner would be for the Kolb cycle to be self-sustaining, but the cycle does require some level of intrinsic motivation unless there is an external facilitator. For a trainee who is burned out, Kolb’s theory may not be relevant as the learner may not have the capacity to tackle a multi-stage learning cycle.
Additionally, while Kolb’s learning cycle shows a continuous progression, in reality, different stages might occur out of order or simultaneously, which can be difficult to predict. It may be useful to lay out Kolb’s learning theory when engaging with a trainee to employ a shared mental model for learning, such as how to approach a new procedure.
Lastly, Kolb’s ELT does not consider the social context of the learning, including power dynamics between teachers and learners.11 If a medical student is fearful of being reprimanded in front of the entire team, they may be less open to sharing experiences or open reflection. Additionally, it does not take into account racial- or gender-based dynamics. A female intern of color might have a different concrete experience than a white male intern. Effects of prior learning experiences are called out in Kolb’s ELT, but they play a large role in shaping learning for a trainee. For example, a learner who has already seen many patients with chest pain during their rotation will have different experiences and reflections than a learner who has seen relatively few patients with chest pain.
A few days later, Jared returns for another shift and eagerly picks up another facial laceration case, this time with a 3-year-old patient.
“Hi Dr. Jones, I have a 3-year-old male with a 2 cm forehead laceration that needs repair. I’ve already discussed intranasal midazolam use with the family and the nurse applied the topic anesthetic. I feel comfortable repairing with your supervision.”
Dr. Jones nods and gestures towards Jared to sit. “I’ve been thinking about the laceration we had together a few days ago.” She wanted to use this clear concrete experience as a discussion point with Jared. Aiming to open the door for reflective observation, she asks Jared: “How did that feel to you?”
“It was really stressful for me because I felt like I didn’t get a chance to try,” Jared replies.
Dr. Jones asks, “What could I have done to help you?”
“Well, I would have liked to have at least tried more than irrigating. But, I don’t think I prepared the family well enough for the sedation. I thought we would knock the kid out! I think I started out on the wrong foot with the family and it seemed like you took over because they were upset.”
Dr. Jones notes that this is a powerful reflective observation. Dr. Jones stands up and motions for Jared to walk with her to the procedural practice area. “I think one part of the issue is that I did not assess your familiarity with the types of sedation we use for pediatric procedures. What I discussed with the family when they were upset is typically how I prepare them for intranasal midazolam use.” (Dr. Jones reflectively observes and initiates abstract conceptualization)
“Yeah, it was useful to be there for that discussion and I used it to model how I spoke to the patient’s family today.” Dr. Jones nods, noting that today’s patient is a concrete experience where Jared can engage in active experimentation.
“That’s good to hear,” Dr. Jones replies. “Let’s walk through your approach in a pediatric patient. We can practice the procedure on this practice suture pad. We can discuss how I prepare families for the repair and when it would be appropriate for me to intervene.”
As they walk through laceration repair, Dr. Jones spends five minutes reviewing her laceration repair checklist with Jared in an effort to engage in abstract conceptualization.
“I hope that was helpful,” Dr. Jones says as they walk back over to the work area.
“To be honest, at first I didn’t think I actually needed to review laceration repair, but I see how it can be different in a pediatric patient. I do feel more prepared and am excited to do this one, but understand clearly when you would need to intervene.” Jared replies. Dr. Jones notes again that Jared is engaging in more reflective observation.
“Okay, gather your supplies, and come grab me when the nurse has given intranasal midazolam and we can do this laceration together,” Dr. Jones states to Jared. She hopes that prepping Jared will not only set him up for success, but also make for a better experience for the patient and family. They are both, in a way, engaging in active experimentation – Jared in his laceration care, and herself in terms of her supervision of trainees.
Annotated Bibliography
1. Kolb DA. Experiential learning: Experience as the source of learning and development. 2nd Edition. Upper Saddle River, NJ: Pearson Education, Inc; 2015.
The first edition (1984) of this book introduced Kolb’s experiential learning theory. This updated edition still contains the original underlying structure behind the theory, while also discussing research supporting the theory over the past 30+ years, addressing concerns with the original publication and displaying current examples of experiential learning both in the field and in the classroom.10
2. Kolb DA, Boyatzis RE, Mainemelis C . Experiential learning theory: Previous research and new directions. In R. J. Sternberg & L.-f. Zhang (Eds.), Perspectives on thinking, learning, and cognitive styles. Lawrence Erlbaum Associates Publishers; 2001:227-247.
This chapter reviews the basics of ELT and how different learning styles fit into them. Learning styles address how learners reconcile conflicts within learning processes, and include accommodating, diverging, assimilating, and converging.2
3. Yardley S, Teunissen PW, Dornan T. Experiential learning: AMEE guide No. 63. Medical Teacher. 2012;34:102-115.
This paper reviews theories behind experiential learning as it relates to medical education, including the background of experiential learning. Importantly, this paper discusses other theories that have added to Kolb’s ELT and points out that in medical teaching, implementation of Kolb’s theory often goes without support at each stage, which can be detrimental to the learner. Support for both learners’ conditions and processes for experiential learning can lead to improved outcomes of the learning.11
5
Authors: Laryssa Patti, MD and Greg Kelly, MBBS
Editor: Michael Gottlieb, MD
Since moving to the city one year prior, Ahmed had developed an outstanding reputation with his medical team. He was older than most of the other fellows, having started surgical training in Syria before making the switch to emergency medicine in the U.S.. Unsurprisingly, his technical skills were excellent, but it was his calmness, humility, and patience that made him so popular with the department. “We love Ahmed” had become a refrain amongst the nurses when they saw his name on the roster after what had been a few legendarily hectic night shifts, even for this hospital. The delicious food that his wife sometimes brought in for everyone only further boosted his reputation.
Ahmed had moved with his family from a smaller regional hospital after failing his first attempt at the board exams. His mentor there, a friend of the medical director, had personally called to recommend him. “Ahmed’s fantastic, he’s not someone we’re trying to get rid of at all. But as you know, the teaching culture here is not what it could be, and you’ve built a great reputation at your shop. Ahmed is clinically excellent and works really well with our team, but he came from a very different system and English is not his first language. I don’t have any doubts that he can pass, but I don’t know if he will from here. I think exposure to your teaching program is what he needs to get him through.”
The boards were a month away and there were a record four fellows sitting. After participating in the local study group for almost a year, Ahmed had become much more comfortable with case discussions in English. He’d been meeting regularly with local mentors to talk over recent articles and had facilitated a great discussion at the local trauma study day, where he demonstrated his deep experience of gunshot wounds. Recently though, this had all been starting to slip. His grand rounds presentation was, frankly, embarrassing and required his co-presenter to step in and save the day. He’d been rude to a surgical attending who he’d called overnight and several nurses had complained about his recent behavior. Kerry, the medical director, didn’t believe in letting things fester. She saw him walk past her open office door and leapt up from her desk. “Ahmed, do you have a few minutes to talk?” He’d been to her office a few times since he arrived. She loved the way he prepared and drank tea in such a fastidious but elegant way. They’d covered all topics from medicine to Ahmed’s hopes for his homeland and his family. He was someone who she and most of the faculty saw as a potential future colleague who would bring great strength and diversity to the department.This time, as he closed the door and turned back to face her, Kerry saw a completely different expression from Ahmed’s usual one. Worry, fear, even anger flashed across his drawn face. She asked Ahmed to sit down and said “Do you want some tea?” What was going on?
Overview
Maslow’s Hierarchy of Needs is a comprehensive theory of human motivation. It attempts to explain all aspects of human motivation by encompassing the full range of needs from those necessary for survival to the need for self-actualization and spirituality. These needs are organized in a hierarchy of “pre-potency”, meaning that basic needs must be met prior to higher level needs being addressed. The lower level needs (in ascending order) include physiological requirements, safety, love, and esteem. The highest levels of the hierarchy include self-actualization, realizing one’s unique potential. In Maslow’s later work, this included transcendence, going beyond one’s self.
Examples of the lower level needs:
If all of these needs are met, the individual can pursue self-actualization, which Maslow defines as “the individual doing what he [or she] is fitted for.”1
Main Originators of the Theory
Abraham Maslow
Other important authors or works:
In 1943, Abraham Maslow published “A Theory of Human Motivation”,1 in which he described the concept of a hierarchy of needs that motivate human behavior. Maslow’s work arose from the humanistic school of psychology, standing in contrast to the behavioralist school. With reference to education, the behaviorist view was that education was a science that involved transmitting knowledge in the most efficient way. In contrast, the humanists took a more holistic view of people and believed that that an educator’s role was to facilitate the growth of their students, enabling them to self-actualize.2
Maslow posited a hierarchical relationship between physiological needs and increasingly sophisticated needs, eventually ending in self-actualization. In his first paper, he grouped the first four needs (physiologic, safety, love, and esteem) as “deficiency needs” (or “D-needs”) because deprivation in any of these categories will motivate behavior to resolve that deficiency. For example, the individual without reliable housing will be motivated to address that deficiency prior to trying to develop an artistic talent as an expression of self-actualization. Additionally, the longer an individual is lacking in a D-need (for example, the hungrier they are), the more motivated they will be to rectify the deficiency (greater effort to find food). In comparison, self-actualization is not driven by a lack of something, but rather by the individual’s need to become what they can be. Hence, this has been referred to as a “being need” (or “B-need”) and can significantly differ from person to person. According to Maslow’s theory, as the D-needs are progressively satisfied, an individual can address needs farther up the hierarchy until, ultimately, they can focus on achieving self-actualization. The processes of learning may be different from the processes required to complete a task.
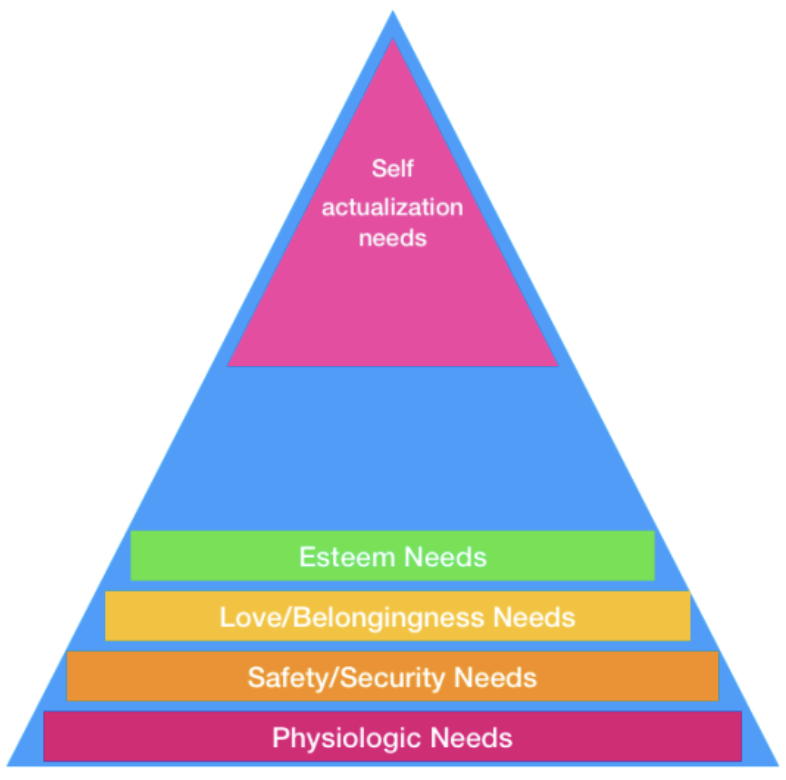
Figure 1. Visual representation of Maslow’s hierarchy of needs. The figure above highlights the various elements of Maslow’s hierarchy of needs (Physiologic Needs, Safety/Security Needs, Love/Belongingness Needs, Esteem Needs, Self-actualization needs).
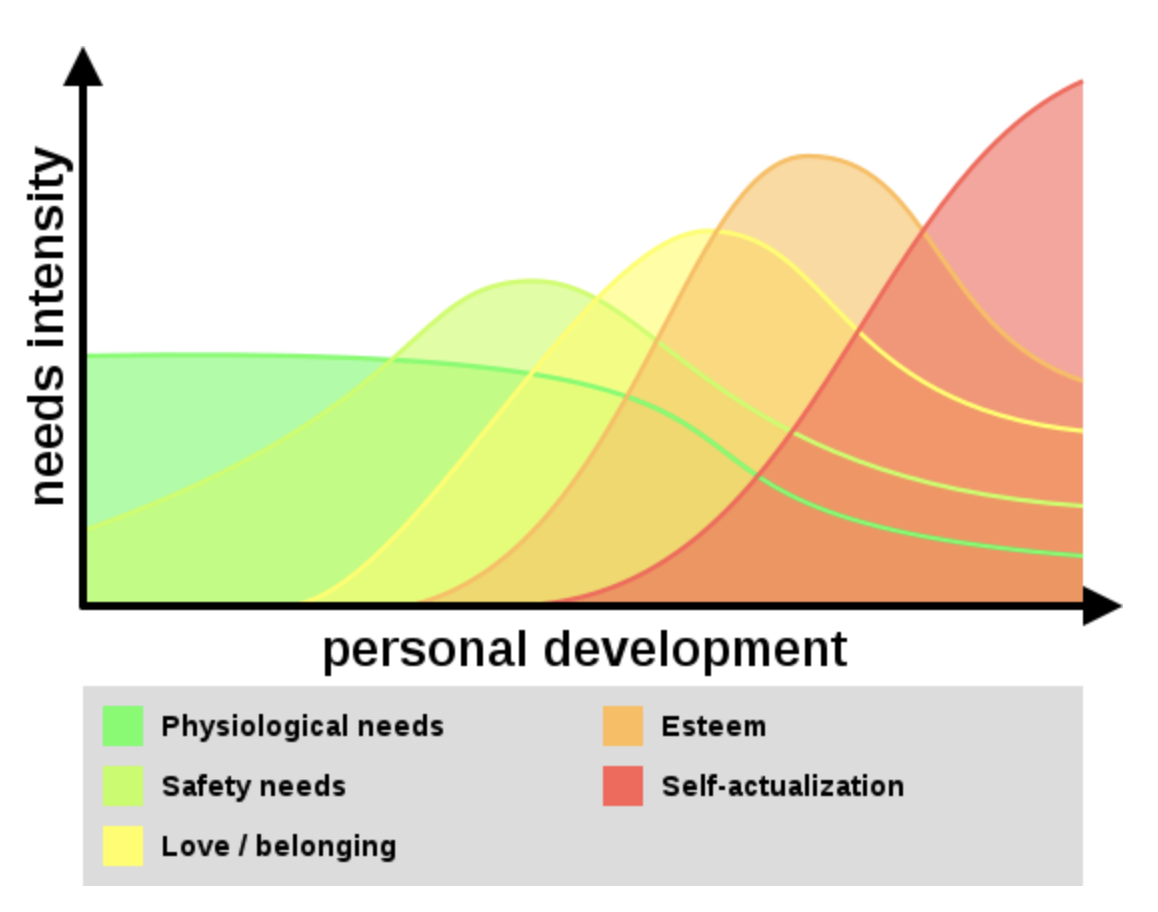
Figure 2. Dynamic trending of Maslow’s Hierarchy of Needs. The figure outlines the dynamic natures between needs intensity and personal development and how it interfaces with the various elements of Maslow’s Hierarchy. From Wikipedia Commons (Used under a creative commons license, CC-4.0-SA).
Later work, including that by Maslow himself,3 de-emphasised the rigid order of needs with the recognition that people do not need to completely satisfy a need before pursuing another, higher order need. Alternatively, he proposed that satisfaction of needs on numerous levels are sought simultaneously.
Herzberg’s two-factor theory of motivation7 arose out of studies of workplace motivation (as opposed to more general motivation theories of Maslow) but there are strong parallels with Maslow’s work. Herzberg’s ‘Hygiene Factors’ align with Maslow’s deficiency needs while the ‘Motivating Factors’ align with Maslow’s being needs. However, Herzberg argued against the idea of needs occurring along a continuum.
The level that esteem, status, and mating-related motives (e.g., mate acquisition, retention, sex, and parenting) should occupy on the pyramid remains a topic of debate. In 2010, Kenrick and colleagues proposed that mating-related motives should replace self-actualization at the top of the pyramid, adjusting the goals of the pyramid with an emphasis on propagation of humanity.8 However, the authors agreed that basic physiologic needs should remain as the base of the pyramid.8
Seventy-five years after Abraham Maslow’s initial publication, there remains no broadly accepted theory of human motivation. Contemporary authors argue for the continued relevance of Maslow’s work because it is widely recognized, continues to place human motivation at the center of education studies, and “resonate[s] powerfully across disciplines,” whilst acknowledging that Maslow’s hierarchy is not strongly supported by modern science.9,10 Self-actualization remains an achievable and desirable goal, as our culture continues to revere those who appear authentic, purposeful in their decisions, and certain in their beliefs and principles.
Since the early 1960s, Maslow’s hierarchy of needs has been incorporated into educational theory. Maslow evaluates the learner holistically, taking into consideration the learner’s physical, emotional, social, and intellectual qualities. It seems apparent that a learner who is unable to address basic physiologic needs would be unable to focus in the classroom. In clinical settings, we must consider whether clinicians have regular access to water, food, bathrooms, temperature control, and an appropriate environment to do their work. How many times have you heard a clinician say that they have not eaten all day because of a busy clinical shift?
A sense of safety may not translate to simply protection from the elements, but rather a sense of security in the clinical setting as well as in the classroom. In the emergency department, this can include the basic protection from violence, ensuring a setting that allows for appropriate patient care with the right tools and sufficient space, and having job stability without fear of being replaced.
Additionally, the classroom should be a place where a student feels like they are a part of the culture and “belong”, as well as a sense that they are esteemed by their classmates and teachers. In the clinical setting, this can translate to a clear role on a patient care team, as well as a cooperative relationship with consultation services and between team members, in which all team members are treated with respect.
In residency programs, the goal should be to train residents who are “self-actualized.” In this context, they should be confident in their ability to perform patient care, be leaders, and advocate for the patient. Self-actualization is unique to the individual, and it is the educator’s role to help the learner along their individual path, rather than molding them in a certain image. The goal should be “to facilitate the student’s discovery and actualization of their nature, vocation, what they are good for, and what they enjoy doing.”2
As educators, if we improve working conditions, this can allow students and residents to focus more on learning and engage them in their quest towards self-actualization.
Due to the nature in which Maslow’s theories were developed, it is difficult to perform replicable testing or validity evaluations. The definition of “need” may be different between individuals. Maslow’s sample set for biographical analysis was skewed, as it had few women, focused on high-profile individuals, and only took into consideration cultures that were similar to his own. Additionally, more recent data has suggested that people are able to establish meaningful relationships and obtain a sense of belongingness, or even self-actualization despite not achieving some of the more “basic” needs as per Maslow’s definition.12
As Ahmed sat down opposite Kerry, he looked up briefly with his tightly-drawn expression and then down at his hands clasped in his lap.
“Ahmed, I’d like to ask you about a few things that have happened recently. I want to start by saying that we really enjoy having you here and value you highly. It’s not easy to win over some of our nurses but you’ve done it. However, in the last two weeks there have been instances where people have found it difficult to work with you or found your communication unfriendly. I’d like to know your side of the story.”
Ahmed, who had been staring somewhere past Kerry’s left shoulder, rubbed his face with both hands. Finally looking up, he sighed. “Doctor Kerry, I am really sorry. I know exactly the times that you are talking about. I have already apologized to each of them and I would like to apologize to you, too. I have been really stressed for the last three weeks as I feel like I am living in a nightmare.”
“My wife has been having trouble with her visa since leaving her engineering job and she has to leave in two weeks. We thought she would get a spouse visa, but the immigration office wants our marriage certificate from Syria. She has tried to get her job back, but she needs a visa. Every time we speak to someone from immigration, we are told different answers. I’ve been spending all day waiting on hold. My boards are in less than two weeks and, if I fail again, my visa might also be in trouble.”
Kerry nodded. “Ahmed, I’m sorry. I can understand that must be incredibly stressful. We had a fellow recently with a similar situation. Fortunately, the college has an incredible immigration lawyer who may be able to help us. Let me call her for you.”
Fortunately, the immigration lawyer (Daniela) was free that afternoon. Kerry told Ahmed to take the rest of the day off and sent him straight across the street to see her. He arrived back two hours later and poked his head around the corner of Kerry’s door.
“Doctor Kerry?” He was smiling.
“Come in, Ahmed. How was your meeting with Daniela?”
‘Fantastic,” he said. “She said this is a common problem and that there is another visa class that we can change to. We have an appointment tomorrow morning with the visa office. Daniela is amazing. I must get back to my shift but thank you so much, I greatly appreciate it.”
He got up to leave but as he reached Kerry’s door he turned back. “Doctor Kerry, there is something else.”“Yes, Ahmed?” “Daniela said that you told her that you needed her help as you wanted me to join the staff once I passed my boards. She said it’s OK to tell me that.”
“We do Ahmed, if that’s what you want. Is it?”“Doctor Kerry, I would love that. I love my job here. My wife and children love this city, too. We feel accepted and peaceful here. I have many ideas about contributing to your amazing team.”
Annotated Bibliography
1. Maslow AH. A theory of human motivation. Psychological Rev. 1943;50(4):370-396.
This is Maslow’s original article, in which he outlined his five levels of needs (physiological, safety, love, esteem and self-actualization) and the concept of pre-potency. In Maslow’s later work, he added ‘transcendence’ as a need above self-actualization, and moved away from the idea of a rigid, sequential hierarchy.11
2. DeCarvalho RJ. The humanistic paradigm in education. The Humanistic Psychologist. 1991;19(1): 88-104.
This is a good article about the work of Abraham Maslow and his contemporary Carl Rogers with particular reference to education. DeCarvalho argues for Maslow’s humanist perspective that an educator’s true role is to unlock the potential of their students and to facilitate their growth, enabling them to self-actualize. To do this, students must be aided in connecting to the purpose, goal, and ultimate value of the acquisition of knowledge. True learning, from this perspective, is possible when it is “intrinsic, experiential, significant, or meaningful.”
3. Kroth M. Maslow – Move aside! A heuristical motivation model for leaders in career and technical education. Journal of STEM Teacher Education. 2007;44(2):3.
This was written primarily for educators in the science, technology, engineering, and mathematics (STEM) fields but is easily applicable to other fields. Kroth argues that there is no universally accepted theory of motivation and reviews numerous theories of utility to educators, while proposing a framework which incorporates the work of Maslow and others. Kroth acknowledges the limitations of Maslow’s theory whilst defending its usefulness, especially as it is simple to understand and recall.
4. Tay L, Diener E. Needs and subjective well-being around the world. Journal of Personality and Social Psychology. 2011;101(2), 354-365.
This was a modern evaluation of Maslow’s hierarchy of needs. The authors surveyed a sample of participants across 123 countries searching for an association between fulfillment and subjective ratings of well-being. This study found that self-reported fulfillment was consistent across cultures, and that fulfillment was independent of subjective well-being even when accounting for socioeconomic status. This study argued that an individual could achieve self-actualization without having all of their basic needs secured first.
6
Authors: Eric Blazar, MD; Vimal Krishnan, MD; Shivani Mody, DO
Editor: Daniel Robinson, MD, MHPE
It’s busy Monday afternoon and the number of patients in the waiting room is only increasing. The attending is paired with a PGY 2 EM resident. Both the attending and resident are completing charts when the triage nurse hastily interrupts stating, “This very nice woman in bed 6 appears to be having a stroke and she’s inside the tPA window.” On impulse, the attending and resident both stand and calmly walk over to evaluate the patient. Before them is a mid-50s appearing, well groomed woman sitting calmly in the stretcher. The resident starts taking the history as the attending observes from the doorway. The patient states that she is experiencing difficulty speaking and left arm weakness while she was at work. Her symptoms began 2 hours prior to arrival.
The resident takes a lengthy and thorough history and performs a physical examination. During the history, the attending notices the patient is having difficulty with word finding, is unable to resist gravity in the left upper extremity and has slight weakness in the left lower extremity. The resident turns to the attending and states that the patient needs an emergent CT scan and places the order in the computer. The attending reminds the resident that a set of vital signs and a point-of-care (POC) glucose are necessary prior to CT scan. Aside from noted hypertension, the patient’s vitals and glucose are appropriate and the patient is taken to the CT scanner. While the patient is in the CT scanner, the attending physician discusses the case with the resident. The attending posits the role of thrombolytics and the resident states that if the CT scan is negative for an acute bleed, thrombolytics may be indicated. The patient returns from the CT scanner and radiologist calls shortly after stating the CT is unremarkable for acute pathology. The attending asks the resident to question the patient about any contraindications she has to thrombolytics. The resident states he is unsure of the contraindications. The attending also asks if blood pressure control is necessary as the blood pressure is 260/130.
The resident states that he is unsure of the blood pressure goals and also states he is not sure how to best treat the blood pressure in this patient, if necessary. The attending starts the patient on a labetalol drip for blood pressure control. 40 minutes have passed since the patient’s arrival and it has been determined by the treatment team that thrombolysis is indicated. After a long discussion with the patient and her family, the decision is made to administer thrombolysis. Now 2 hours and 50 minutes following onset of symptoms, the resident sits down to order the medication and states to the attending that he is not sure what the dosing is or how thrombolytics are administered. The attending places the order. Following administration, the patient is admitted to the critical care/neuro intensive care setting at the hospital. While both the resident and the attending are charting, the attending physician asks the resident to reflect on the case. The resident tells her, “I’ve really only ever taken care of one or two acute stroke patients and today was my first time administering thrombolytics. I feel like I know a lot about stroke but I’m just not comfortable managing it in the ED.”
Overview
Multiple studies in medical education have demonstrated that performance on examinations does not reflect proficiency in patient care. That is, strong written test performance demonstrating a strong grasp of medical science knowledge does not necessarily translate to excellent patient care.3
Miller’s Pyramid provides a framework for assessing clinical competence in medical education beyond test-taking or memorization. The pyramid, sometimes called Miller’s Triangle, can also assist clinical teachers in matching learning outcomes with expectations of learner performance at specific training levels. The framework, shown in Figure 1, starts with the wide base of “knows” representing knowledge. The pyramid transitions up to “knows how” or competence. Next, “shows how” is demonstration of performance. Finally the ultimate point of the pyramid is “does” or action. Miller’s pyramid demonstrates the importance of having more than just medical knowledge, emphasizing that delivery of care is necessary for excellence in medicine.1 The pyramid focuses on the importance of acquiring knowledge to perform a task in practice.4 It also presents a standardized step-wise approach to clinical pedagogy and trainee assessment.1
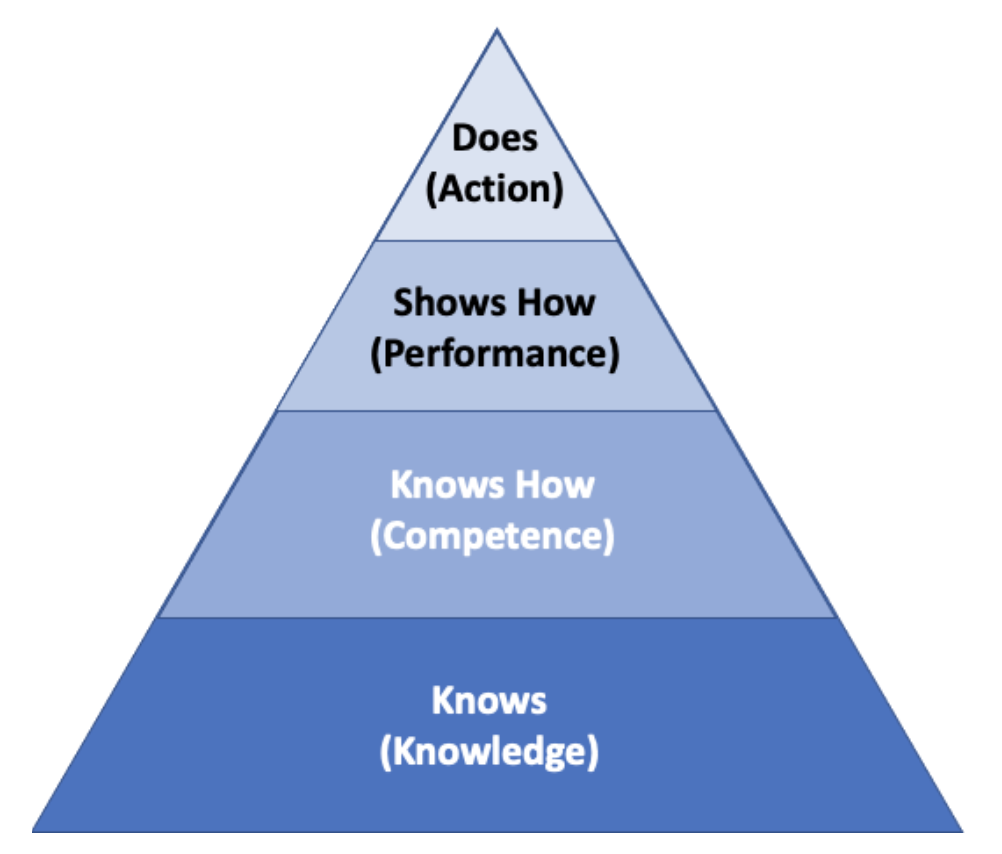
Figure 1. Miller’s Framework for Clinical Assessment. George Miller’s framework is often represented as a pyramidal structure that shows the framework beginning with “Knows” (Knowledge) at the base, and then progressing to “Knows How” (Competence), “Shows How” (Performance), and “Does” (Action).
Main Originators of the Theory
George Miller
See: Miller G. The assessment of clinical skills/competence/performance. Academic Medicine. 1990;65(9):S63-7.
Created in 1990 by George Miller,1 Miller’s pyramid (Figure 1) was initially created and utilized as a framework to clinically assess trainees at varying levels.1 Starting with “knows”, the base of the pyramid is based on knowledge and Miller opines is the easiest to assess. Simply, standard medical knowledge is tested through board examinations and medical school testing. These tests are considered incomplete assessment tools in Miller’s view as he states in his original opinion piece that medicine requires more than scientific knowledge to master excellence in medical care. In essence, Miller emphasizes the art of medicine. Miller views knowledge as the introductory and basis for clinical competence. Learner knowledge (”knows” stage) about tube thoracostomy, for example, would be the ability to state indications and contraindications for placement or demonstrate understanding of the pathophysiology of congestive heart failure (CHF).2
The second stage of the pyramid is “knows how”. This is the assessment of the ability to analyze and interpret the data obtained or as Miller classifies, competence.1 Competence can be assessed by testing on simulated patients or performing procedures in simulation. The US Medical Licensing Examination (USMLE) clinical skills (CS) assesses this second pyramid level of competence. The learner in this phase is able to describe the steps in placing a chest tube or discuss the steps in managing CHF.2
The third stage is “shows how”. Miller describes this as assessing the performance of the learner in clinical situations. Performance assessment is the learner’s ability to apply knowledge and to analyze data when faced with a patient situation.1 Rather than working through the physical examination on a standardized patient as in “knows how”, standardized patients can be used to ascertain not only data gathering but formulation and processing outside the clinical setting. Other attempts at assessment of clinical performance are Objective Structured Clinical Examination (OSCE) and Mini-Clinical Evaluation Exercise for trainees (Mini-CEX).2 Assessment on the hospital wards by clinical teaching faculty fall under the performance assessment. However, Miller cautions against this “shows how” type of assessment as he states there is declining direct observation of the learner and most of the learner skills are interpreted during rounding or discussion of disease etiologies.1 In the 1960/70s, studies found bedside teaching and direct observation of the learner occurred in about 75% of patients. In contrast, Gonzalo et al in 2009 found a sharp decline in bedside direct observation teaching, occurring only in about 25% of precepted patients.11 Stickrath et al found in their study, “Teams infrequently … taught physical examination skills (14.6%), evidence-based medicine topics (7.2%), or learner-identified topics (3.2%). Many commonly performed activities occurred infrequently at the bedside.”11 With this move away from direct involvement and observation by the educator, Miller opines that assessment of the learner in their ability to “shows how” is mere inference.
The apex of Miller’s pyramid is “does”. “Does” represents action and assessment of the physician’s ability to function independently in the clinical setting.1 Miller discusses that this is the most difficult to measure. Current attempts to measure action in the clinical setting include patient satisfaction surveys, demonstration of post procedure care and other aspects including functional status, cost effectiveness and intermediate outcomes.2,7
Miller’s pyramid presents a graded method of assessment for learners. In 1990, he was suggesting a paradigm shift hoping to refocus medical education and stress the importance of assessment outside of just knowledge. In today’s medical education ecosystem, Miller’s pyramid aids in understanding the question we are testing and insures the assessment is valid.
Since 1990, Miller’s idea has been adapted to continue to fit the changes in the field. As Miller hoped from his original opinion piece, medicine has changed paradigms with a marked greater focus on teaching the art as well as the science of medicine. As the learner familiarizes themselves with concepts and skills, there is understanding that comes before having strict knowledge of the subject. Two underpinned awareness levels, “heard of” and “knows about” have been added to Miller’s pyramid below “know”. (Figure 2) For instance, knowing of a chest tube but not knowing the indications for placement is a precursor knowledge set.6
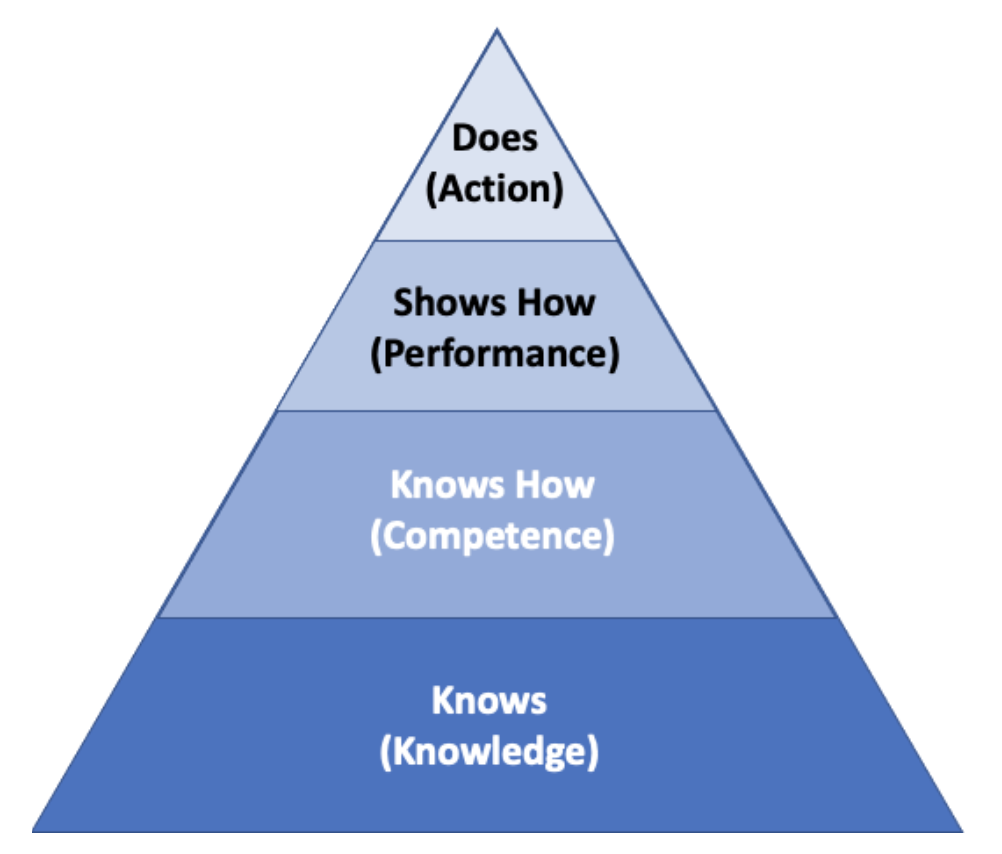
Figure 2: An adaptation of Miller’s Pyramid adding “Knows about” and “Heard of” below the other levels.
Cruess et al added a fifth level above “does”. “Is” should reflect not only clinical competence but the presence of a professional identity.8 Medical education evolved to consider the “attitude” part along with knowledge and skills, which is reflected in Miller’s prism (Figure 3). This adds a third dimension of professional authenticity onto the original Miller’s Pyramid. Professional authenticity focuses on “attitudes”, “skills” and “knowledge” on a spectrum of novice to expert. Thus, “does” with expert level attitude, skills and knowledge is the apex of Miller’s prism which was remodeled in 2009, nineteen years later.6
Rethans et al. recognized that both internal and external factors influence performance and wanted to further focus on “performance-based assessment measuring what doctors do in actual professional practice.”9 Thus, the Cambridge model was created as a modern adaptation of Miller’s pyramid.9 Beyond the apex of the pyramid, “does” or competence, both system and individual related influences will affect physician performance. System influences consist of any driving factor affecting or being dictated by the community. These influences consist of guidelines, government programs, time available to spend with patients and even patient expectations. All these factors influence a physician’s daily performance. Test utilization and adherence to guideline metrics are attempts to measure daily performance. Individual influences, such as personal and mental health and occupational relationships, will also influence the physician’s overall performance.3,8 Thus, Rethans states that one’s individual competence plus individual and system based external forces come together to dictate a physician’s overall performance.
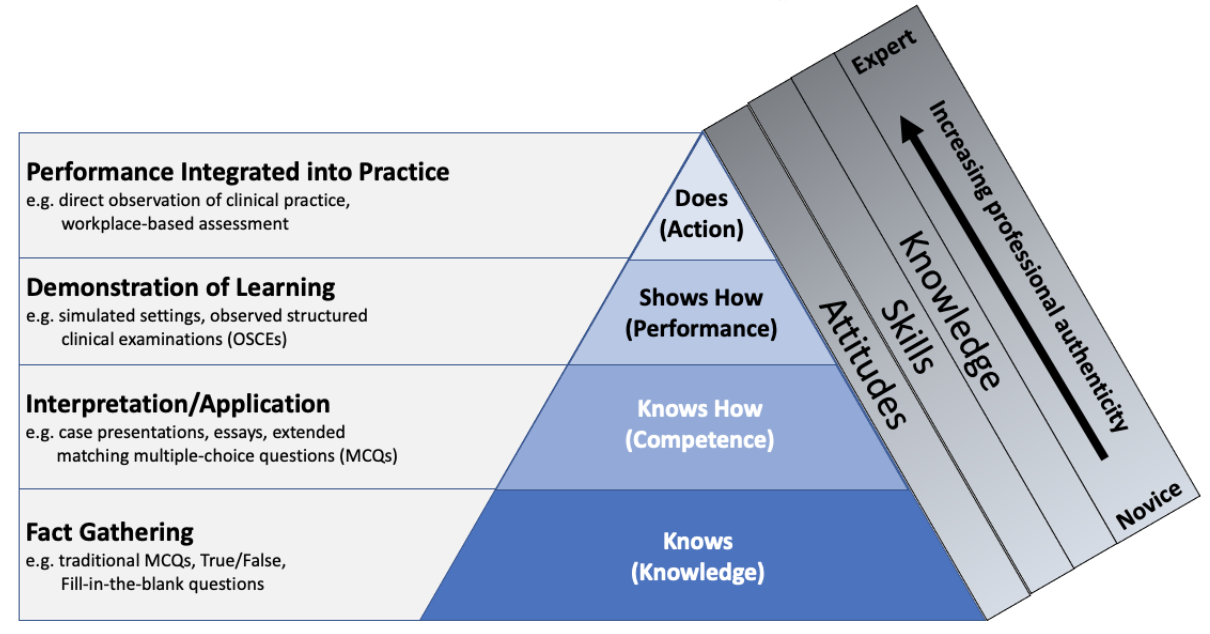
Figure 3: Medical education evolved to consider the “attitude” part along with knowledge and skills, which is reflected in Miller’s prism.
Miller’s pyramid can be used as the transition from classroom to clinical setting. As constant learners of new knowledge, physicians are always maturing through the pyramid from “knows” to “does”. While on a grander scale, practicing medicine is a competency that has been divided into specialities, Miller’s pyramid can also be used on a much smaller level. Starting on a large scale in the US, medical students select and match into residency programs and then test in many various ways and gain board certification for a specialty or multiple specialty practices. Individual practice and board certification are progressions up the pyramid as one becomes able to clinically demonstrate mastery of a medical specialty. However, on a smaller scale the pyramid becomes applicable for new knowledge physicians gain at conferences or through other continuing education to update their skills. For instance, if an older attending uneducated in ultrasonography that already performs at a “does” level attends a workshop to develop ultrasound competency, that provider will progress up the assessment levels of the pyramid through testing, then observing and then on shift quality improvement as they improve and increase their image acquisition skills. Thus, assessment must be separated into graded measurable goals for various skills and knowledge bases as skill mastery progresses for providers.
While Miller’s pyramid has become widely utilized as the basis for benchmarking training assessment and performance, as with any education theory, Miller’s pyramid does have some limitations. First, Miller himself notes the difficulty in assessing “does”. To assess physicians in their work environment while they are actively treating patients is challenging, expensive and time consuming. The underlying test/observation would never be the same for two different providers as no two patients, patient encounters, or care environments are the same. Thus, comparison becomes quite difficult when evaluating proficiency at the top of the pyramid.3,7 As case mix and number of cases vary, complexity and attribution also contribute to the complexity of measuring. Physicians are not the sole dictators of patient outcomes and thus only monitoring outcomes is inherently flawed.3,7 However, at this time in health care, patient outcomes seems to be how physician proficiency and assessment is monitored.3
The pyramid is based on the assumption that assessment in actual practice environments is a better reflection of routine performance as opposed to preset/ artificial testing conditions.7 While this framework is widely accepted, Miller even notes in his original manuscript that he is basing his pyramid on conjecture. He assumes that observation in reality is a more effective truth than simulated or testing environments.
Miller’s pyramid also is limited in that it assumes that competence predicts performance. Demonstrating competence in the “does” apex of the pyramid is assumed to predict future good performance. Often times, there are other influences on one’s performance. A physician or learner’s performance can be greatly dictated by availability, time, energy level, mood, the environment and the patient.4
After the attending recognized the resident’s significant knowledge gap in the management of acute thrombotic stroke, the attending provided feedback to the resident the following day in an email stating that his history was too extensive and delayed the patient’s CT scan. He also forgot to obtain vital signs and a POC glucose. He was unable to manage the patient’s blood pressure and was unsure of many of the contraindications to thrombolysis administration. The attending provided this feedback in a constructive and non-threatening manner and provided resources from EM text books as well as a link to a video lecture and a podcast to augment the resident’s learning. The attending was focusing on moving the learner from “knows” to “knows how”.
One week later during EM didactics the resident approaches the attending stating the resources were excellent and he feels much more confident in his acute stroke knowledge. The attending offers a simulated case as practice to the resident. Later that day in the sim lab, the residents goes through 2 cases of acute thrombotic stroke and displays his comfort with his new knowledge. The attending is very pleased with the resident’s improvement and the learner has moved to “shows how.” During the debriefing from the simulation, the attending talks about the limitations of simulation as well as the need for continued assessment of the resident when managing acute CVA patients in the ED. They develop a way for the resident to ask the attendings for attention and feedback when managing other acute stroke patients on shift in the ED.
Annotated Bibliography
1. Miller G. The assessment of clinical skills/competence/performance. Academic Medicine. 1990;65(9):S63-7.
Miller’s original manuscript where he presents his pyramid for clinical assessment. (Knows, knows how, shows how, does). Miller suggests that testing is antiquated and not getting to the center of necessary assessment. He suggests that while testing knowledge is important, an advanced learner must know how and then show and finally do. He suggests different manners for assessment at each level of the pyramid.
2. Rethans J, Norcini J, Baron-Maldonado M et al. The relationship between competence and performance: implications for assessing practice performance. Med Educ. 2002;36(10):901-909.
Rethans et al further expanded on Miller’s pyramid of assessment and further theorized that competence is not solely influenced by performance. Rethans demonstrates how there are both systemic and individual external factors that play significant roles in influencing perceived and observed competence. Systemic influences include any determinant from the governing body or hospital of employment as well as government influences on health care. Individual influences, such as provider wellness and health, mood, patient mood and wellness, among many others also equally play a role in performance and thus competence. Rethans decided that an inverted pyramid would best show that performance is based on competence as well as systemic and individual influences equally.
7
Authors: Matt Zuckerman, MD; Alison Hayward; MD, MPH
Editor: Benjamin Schnapp, MD, MEd
Matt is an Emergency Medicine intern preparing for this week’s conference. He attempts to watch one of the suggested Free Open-Access Medical Education (FOAM) videos about diabetic ketoacidosis (DKA) while washing the dishes and keeping an eye on his 12-month-old daughter. He finished the video twice but each time he finds that he can’t remember anything. Matt feels frustrated because he knows that he’s attempting to do three things at once and doing them all poorly. Between his clinical responsibilities and trying to keep things going around the house, he rarely gets time alone to study. He’s worried that the only option is going to conference unprepared, neglecting his daughter, or switching to take out meals. He ponders his dilemma and realizes that the main issue isn’t necessarily needing more time, but figuring out some way to process everything more efficiently.
Overview
Multiple resource theory attempts to describe the demands placed on an operator simultaneously performing multiple tasks. Why is it easier to do some things simultaneously, while others interfere? Why do we turn down the radio when we’re lost in the car but not when we’re eating? The difference lies in how much processing each activity requires and whether they require similar resources. Tasks that require high levels of processing or similar resources (input channels, motor responses) will be done less efficiently simultaneously. Improved efficiency can be obtained by separating the overlap.
One example is pulse oximeters that warn of low oxygen levels or pulse rates with changing audio tones while an operator is looking at an airway and using muscle memory to place an endotracheal tube. Our brain localizes processing of different media to various areas (vision in the occiput, auditory processing in the temporal lobe). As such, we can monitor visual and auditory channels simultaneously without a serious degradation in efficiency. Researchers have demonstrated that brain lesions localized to the visual cortex vs the auditory cortex can have divergent effects on processing pictures vs sounds. The example of the pulse oximeter uses these divergent pathways to increase the amount of information we are able to process simultaneously.
The degree of processing required is a result of task complexity or operator experience and also has an effect on the example above. An experienced intubator notes a grade 3 view of the vocal cords and immediately adjusts the laryngoscope to improve to a grade 1 view. This muscle memory is gained through countless hours of consciously adjusting the laryngoscope to see whether raising or lowering the blade improves the view. Those same hours may be spent learning to drive. A student driver will have difficulty talking and driving simultaneously, but an experienced driver will have little difficulty. Alternatively, the experienced driver can safely listen to the radio but would be foolish to watch a movie while driving.
Christopher Wickens, the originator of multiple resource theory, lays out the principles that define multiple resource model architecture: demand, resource overlap, and allocation policy. These principles are used to change the characteristics of the particular activities that are being done simultaneously. These characteristics can include stages of processing (encoding inputs, processing them, responding), modalities (visual or auditory), responses (manual or vocal) or coding (spatial or verbal).1
Main Originators of the Theory
Christopher Wickens
Other important related authors or works:
Christopher Wickens created the multiple resource theory model to explain why some tasks are easier to do simultaneously (walking and chewing gum) while others are much harder (talking and reading). He recognized that several different schools of thought were attempting to explain the same phenomenon in different ways.
Historical explanations of dual-task performance relied on the mechanical analogy of workload and power. As computers became more popular, the conception of learners having a central processor also became popular. Kahneman’s 1973 book, “Attention and Effort,” attempted to explain human performance using a general pool of mental “effort” without differentiated resources.2 Other scientists in the field (Isreal, Wickens, Chesney, & Donchin) noted that resources seemed to be specialized, as the nature of simultaneous tasks affected our ability to do them. In an expansive review of the literature, Wickens attempted to reconcile these theories and integrate the experimental literature.
Wickens posited that tasks compete for a shared pool of resources. Simultaneous tasks that require similar resources may interfere with each other (e.g. reading a book while listening to another book). Performing two tasks simultaneously will usually reduce the efficiency of each task, however this effect is not the same for every task or every operator. In general however, tasks are easier to perform and most efficient when done without competing demands. Even listening to music (which requires few cognitive resources) while driving creates occasional moments when the driver is focused on the music to the exclusion of the road, or is focused on navigating and misses part of a song. In a multitasking scenario, the reduction in efficiency resulting from performing any given tasks simultaneously is known as task interference.3,4
The modern ubiquity of mobile phones increases the tendency to multitask as we constantly respond to texts or lookup information while driving, walking, or engaging in live meetings. This ubiquitous source of work and pleasure is an unanticipated driver of multitasking, not conceived of when Wickens wrote his paper in 1981.
Based on experimental testing of multiple resource theory, Boles has suggested adding tactile input (haptics) as a separate modality of input apart from visual and auditory. For example, pilots that are focusing on a visual display and listening to audio instructions perform better with tactile warnings communicated with vibrations than with visual warnings. These researchers point out that tactile input is an underutilized modality in the design of safety alerts, which tend to rely heavily on visual attention.9 Boles additionally differentiated the auditory and visual processing modalities, breaking auditory processing into “linguistic” and “emotional” components, and visual processing into “positional spatial” versus “quantitative” components. For example, reviewing recent lab values in chart format likely requires different visual resources from reviewing a spreadsheet of numbers.10,11 Practically, this means we can actually process more information simultaneously if we more effectively understand how to separate the input channels. Cognitive load has also been found to occur in potentially unexpected places. For example, it has been observed that visual information can create more interference based on distance in space. If information must be gathered from different sources that require only eye movements, this would cause a lower level of visual interference than information that requires head movement to acquire.8
Other Examples of Where this Theory Might Apply
This theory has important implications for medical education as learners are frequently asked to perform multiple tasks simultaneously. Consideration should be given to multiple resource theory when planning any lecture or workshop, in order to optimize the use of inputs while minimizing task interference for learners. For example, any potential distractions should be avoided while learners are heavily cognitively engaged with learning a new procedural skill, as learners will have few cognitive resources to spare. The theory also supports the idea of multimedia education, as communicating information through different channels helps learners activate multiple areas of the brain and avoid cognitive overload.
Multiple resource theory can also help explain the task efficiency learners gain when procedural tasks become more automatic and require less processing. The surgical intern who must focus solely on tying her knots becomes the senior who can tie knots effortlessly while monitoring bleeding and case progression. It can also help explain why the ED provider can passively monitor the ambient audio conversations of the charge nurse and simultaneously visually review the CT scan on a trauma patient.
Modern high fidelity simulation design should factor these concepts into simulations. Requiring a provider to handle multiple patients at once or monitor vital signs while EMS gives report reflect the demands on multiple cognitive resources that are placed on a provider in the real world. Simulating scenarios in which interruptions in care take place helps trainees to practice and improve on handling and prioritizing multiple types of input at the same time. Studies suggest that high stress and high cognitive load situations with frequent interruptions may result in significant medical errors.12, 13, 14 Through simulation exercises and through senior shifts acting as attending physicians, residents can develop strategies to manage and decrease the cognitive load and optimize their multitasking abilities.
The model also has important implications for clinical practice and contributes to how we present information on patient monitors and in electronic medical records. Design of safety-related alerts must take into account that using different resources will likely increase staff responsiveness to a potential error or problem. For example, some monitors use flashing lights, rather than just auditory stimuli, to indicate a concerning event. Using tactile vibrating phones that specifically alarm for critically ill patients could increase responsiveness when compared to adding yet another beeping machine to the hospital environment. Color-coding labs or vital signs that are abnormal or providing the option of displaying values in a graphical format helps to highlight the abnormal values by engaging different parts of the brain and increases likelihood of providers taking note and responding appropriately.
The limitations of multiple resource theory include variability in measuring efficiency of tasks, as well as the challenge of estimating a ‘baseline’ level of demand for tasks, since the level of demand for a given task may be very reliant on the experience level of the individual in question with the task.15
The multiple resource model assumes that resources will be deployed logically and optimally towards each task being completed. More recent studies suggest that this may not be the case: there are tasks which are more engaging than others, such that they override other tasks. Studies have found that drivers became so engrossed by cell phone conversations that they failed to continue to pay attention to their surroundings, despite the fact that there is little overlap in resource allocation between the two tasks.3,16,17
Matt realizes that he is struggling to process visual inputs from his FOAM video while simultaneously looking at the dishes and his daughter. He instead finds an audio FOAM resource on DKA that he listens to while singing to his daughter about DKA and washing the dishes. In this way he separates visual from auditory inputs and reduces his mental load thinking about what his daughter is doing by entertaining her with a fun song. He also reinforces the material he is learning through simultaneous repetition. By the time he is done with the podcast, the dishes are clean, his daughter is ready for bed, and he is prepared for his conference small group on DKA.
References:
Annotated Bibliography
1. Wickens CD. Processing resources in attention. in Parasuraman R and Davies R, eds. Varieties of attention. New York, NY: Academic Press,1984.
Wickens’ seminal paper on multiple resource theory discusses historical views of the source of variance in time-sharing performance and the formulation of a “performance resources function” that describes the relationship between the quality of performance and the quantity of resources invested in a task. The applications of multiple resource theory are detailed in practice.
2. Wickens CD. Multiple resources and performance prediction. Theoretical issues in ergonomics science. 2002 Jan 1;3(2):159-77. The theory is approached from the perspective of its predictions for task interference dependent on the cognitive modality used. For example, will reviewing a map while driving affect the operation of the vehicle and will placement of that map on a heads up display modulate this interference? The multiple resource model is reviewed in detail, with a focus on how the components of each dimension of the model may affect one another in either creating or avoiding task interference, thus affecting time-sharing ability, and, ultimately, performance.
3. Wickens CD. Multiple resources and mental workload. Human factors. 2008 Jun;50(3):449-55.8:
In this paper, Wickens details the origins of the multiple resource theory. He describes additional research done since his seminal paper on the subject and how it has bolstered as well as challenged the theory. He describes the related but distinct concept of mental workload, reporting that the multiple resource theory is most relevant to performance breakdowns related to dual-task overload. Multiple resource model architecture consists of three components: demand, resource overlap, and allocation policy; whereas, mental workload focuses mainly on demand regardless of whether there are multiple tasks occurring.
8
Authors: Meenal Sharkey, MD FACEP, Mary Bing MD, MPH, Kimberly Schertzer, MD
Editor: Anne Messman, MD, MHPE
A new intern is managing a patient with hypotension and tachycardia. The patient is ill-appearing but alert and conversant. The intern recognizes that this is a sick patient in shock. Her attending asks her what type of shock she thinks this is, as each type of shock is managed somewhat differently. The intern is feeling overwhelmed, and the only type of shock she can think of is septic shock. She understands that the definition of shock includes inadequate end-organ perfusion, but she has difficulty coming up with other types of shock (e.g. hypovolemic, cardiogenic, neurogenic). The attending is wondering how best to utilize this situation as a teaching opportunity for the intern to learn other types of shock.
Overview
From the field of Cognitive Science, prototype theory is based on a conceptual organization for categorizing various items based on common features. A prototype is “an original model on which something is patterned.”(Merriam-Webster Dictionary) The features of a prototype are not necessarily defining features, but more of a resemblance that can be related to all the items within the family. If a prototype were placed in a family tree, it would be at the top and everything would descend from that prototype. In contrast, classical theory requires that all items meet a distinct criteria for membership in a particular group. That is, it either belongs or it doesn’t. The boundaries for membership are distinct. To be in the category, it has to be clearly defined and mutually exclusive. In prototype theory, the boundaries can be “fuzzy.”1
In prototype theory, some items resemble a “prototype” more than others. There is not usually a single defining feature that is required for an object or idea to be included in the grouping, but certain objects and ideas “embody” the classification more so than others. That is, the most central member serves as the best example of that category. For instance, under the classification of “clothing,” the item of a shirt more often embodies this concept than say, a cumberband, however a cumberband would still be included within this grouping.2 Within the realm of educational theory, prototype theory also can represent organization of ideas that have shared characteristics.3
In medicine, patients present with a chief complaint or constellation of symptoms rather than a definitive diagnosis. For example, a patient might complain of a bloody cough. We know the differential diagnosis for bloody cough is broad and can include pneumonia, malignancy, pulmonary embolism or tuberculosis, to name a few. Let’s presume we use classical theory and assign “bloody cough” to the pulmonary embolism category. Then you could only have a pulmonary embolism if you also had a bloody cough. We know this would cause us to miss potentially serious causes of disease and potentially misdiagnose or mismanage the patient. Since, in reality, one symptom can fit into multiple categories, prototype theory lends itself better than classical theory to develop a concept of disease categories in order to facilitate the learning and problem-solving process in clinical decision-making within medicine.4
Main Originators of the Theory
Eleanor Rosch
Prototype theory was first proposed by Eleanor Rosch in 1973 after studying how the Dani people in New Guinea classify colors. Their language does not include specific names for colors and instead categorizes them on a spectrum of dark/light or cool/warm. However, they were still able to communicate their ideas of color despite the lack of exact names for colors. This inspired her to investigate how different cultures categorize different ideas. 7, 8 Thus, the prototype theory was formed. This was in contrast to the classical theory of categorization, which involved defining features to rule in or rule out resemblance. The prototype theory takes a clustering approach with the central idea/theory serving as a prototype; radially affiliated concepts can closely or loosely resemble the prototype. This concept addressed an inherent problem within classical theory: often times, definitions were not always agreed upon.
Within the prototype model, even loose associations are tolerated, allowing a broader range of concepts to be included. One large benefit of the prototype theory is that retention often increases as there is a graded concept of relatability2. An interesting aspect of prototype theory is that it can be applied to many different fields including psychology, linguistics, mathematics, medicine, philosophy, and even quantum physics. One of the most recent advances in this theory involved application within the field of quantum physics; mathematical quantification was used to define “data on conceptual combinations.” This application attempted to quantify the “relatedness” of various concepts that were radially related based on the prototype theory.
Modern takes on this Theory
In medicine, Bordage et al4 performed experiments which demonstrated that learning medical concepts is easier when key disorders are studied within a category and then extrapolated out, rather than learning every single diagnosis within a disease category. Papa et al6 found that use of prototype theory can improve medical student diagnostic abilities and can be used to develop student clinical skills with a carefully designed curriculum.
Other Examples of Where this Theory Might Apply
One limitation of this theory is related to the lack of defining characteristic that unifies a particular family of concepts. This can make the associations seem nebulous and ill-defined. Secondly, the organization of concepts is specific to an individual and sometimes even specific to a culture.9 For example, asking someone to categorize various fruits might be different in Africa compared to Northern Europe. Or, alternatively, categorizing various types of clothing would be different in India and in Brazil. Another limitation includes the requirement for a shared, minimal foundation of knowledge. If the original properties of an idea or concept aren’t agreed upon, it will not be possible to link them through groups using prototype theory. For example, in the initial vignette, if the intern did not know what shock was, then there would be no initial starting point from which to break shock down further. Also for diseases that are very unusual or rare, it may be difficult to come up with a diagnosis when it’s so dissimilar to a set prototype.
The intern is overwhelmed by caring for the sick patient and trying to come up with other causes of shock. Her attending reminds her of the other types of shock, and while septic shock might be the “prime” example of shock (due to high prevalence in clinical practice), there are characteristics of each of the other types of shock that make them all recognizable under the umbrella of shock. After the patient is stabilized, the intern has now learned to classify the other types of shock, but as she is most familiar with septic shock, it serves as the “prototype” of shock for her learning. She relates all other types of shock to this example, and notes their differences and similarities. This allows her to learn additional concepts of shock by using a pre-existing framework. As her attending, you determined her “prototype” for a clinical concept to assess the basis of her understanding as the starting point for the other types of shock. This can help solidify the intern’s understanding by starting with a concept the intern is familiar with and expanding on related concepts.
Annotated Bibliography
1. Aerts D, Broekaert J, Gabora L, Sozzo S. Generalizing Prototype Theory: A Formal Quantum Framework. Frontiers in psychology. 2016;7:418.
This paper attempts to mathematically quantify the relationships between words and concepts. One of the challenges is the “creative flexibility” that is inherent to the prototype theory. This paper was interested in the “conceptual distance” between the example and the prototype. This paper is a summary of the mathematical advancements in capturing the framework of concepts within the prototype theory and the interplay between them. The authors developed an approach called the State Context Property (SCoP) formalism. They used participants to assign “membership weights” and “typicalities” to certain concepts and derived equations to show this likeness. Advanced quantum mechanics were utilized to further assess these relationships. This paper was interesting as it attempted to mathematically distill the many variables that go into defining and quantifying what appears to be an inherent relationship within human language. It also showed modern day application to a learning theory that has been around for decades.
2. Bordage G, Zacks R. The structure of medical knowledge in the memories of medical students and general practitioners: categories and prototypes. Med Educ. 1984 Nov; 18(6):406-16
This paper conducted four experiments on preclinical medical students vs experienced general practitioners: 1) “to determine whether the concept of prototypes is applicable to the structure of selected categories of medical disorders as stored in physician memory,” and 2) “to describe to influence of clinical experience on these structures.” This study finds that Prototype view and memory of categories of disease were found in both the preclinical medical students and experienced doctors despite a disparate amount of training. This paper further suggests that medical educators should design medical school curriculum with Prototype theory in mind.
3. Papa FJ, Li F. Evidence of the preferential use of disease prototypes over case exemplars among early year one medical students prior to and following diagnostic training. Diagnosis (Berl). 2015 Dec 1;2(4):217-225
Diagnostic accuracy is difficult with the ill-defined nature of human diseases when individuals can have different signs and symptoms for the same disease process. The authors conducted studies on first year medical students through the use of Exemplar and Prototype theories (System I thought processing) to formulate a training exercise in order to improve their diagnostic accuracy and also to determine if Exemplar or Prototype theory is used preferentially for diagnosis. The authors conclude that the training exercise improved the students’ diagnostic acumen and found that they preferentially used Prototype over Exemplar theory for diagnosis.
9
Authors: Annahieta Kalantari, DO; Eric Lee, MD; David Zodda, MD
Editor: Simiao Li-Sauerwine, MD, MSCR
Melissa is a new emergency medicine intern. Her medical school grades and evaluations were excellent and she is well-liked by colleagues, faculty, and staff. However, since starting residency, Melissa has struggled with regard to her clinical performance.
After some critical shift evaluations, her residency director meets with her. When asked what abilities and characteristics make a good doctor, Melissa has a hard time coming up with specific attributes. She states that learning was easier in medical school as she was able to monitor her success through her performance on regular quizzes and exams. Now, in residency, there are no grades and the expectations are higher. She wants to step up and succeed but she is not sure where to start.
We can all relate to the difficulties Melissa is facing. Many of us can also relate to the challenges her residency director faces as they work to help Melissa achieve her goals. In this chapter, we will take a look at education theory and take a deep dive into the key elements of self-regulated learning. We will discuss how self-regulated learning techniques can be utilized by both residents and educators to achieve their academic goals.
Overview
Self-regulated learning theory is the process by which learners modulate affective, cognitive, and behavioral processes throughout a learning experience to reach a desired level of achievement.1 It was introduced by Zimmerman in 1989 as an integrated theory that addressed the interaction of cognitive, motivational and contextual factors.2 It is made up of three basic components: regulatory agents, regulatory mechanisms and regulatory appraisals.1 Each of these components are described in detail below.
Main Originators of the Theory
Barry J Zimmerman PhD
Other important authors or works:
Self-regulated learning theory is often confused with metacognition and self-directed learning. Metacognition was first introduced by Flavell and described as thinking about one’s own thinking. Although this is an essential component of self-regulated theory,3 it differs in that self-regulated theory incorporates knowledge of cognition in addition to self regulatory mechanisms and self efficacy. Moreover, self-regulated learning theory differs from self-directed learning because in self-regulated learning, instructors provide a scaffolding and guidance for learning. In self-directed learning, the process is entirely learner independent.2
Regulatory agents
The first stage of self-regulated learning is the planning phase. This is primarily done by setting goals. Goal setting is most effective when goals are specific, individuals are committed to reach them, individuals possess task knowledge, and individuals receive feedback on goal progress.1 In Melissa’s case, her medical school goal was to score well on exams. She was able to develop study plans, sustain motivation, and assess her progress in achieving goals with each exam. Her residency goal is to be a good doctor. This is not specific enough. Because it lacks specificity, she is unable to develop an effective learning plan and is unable to assess her progress effectively.
Regulatory mechanisms
Regulatory mechanisms are under the control of the learner and are the crux of self-regulated learning. They are:
As learners engage in goal achievement, self efficacy will redirect which regulatory mechanisms should be incorporated or require adjusting.1
Regulatory appraisals
Regulatory appraisals involve determining where a learner is in the goal achieving process and identifying which factors are contributing or preventing goal achievement.
There are three main components of regulatory appraisal.
The emergence of FOAM and digital resources have the potential to greatly contribute to self-regulated learning theory. Traditionally, learners read through textbooks and deciphered what was relevant and essential to learning. Blogs and podcasts attempt to curate essential information. Online testing resources allow learners to independently assess their medical knowledge progress as well. What FOAM cannot provide are the essential steps of the planning phase but this can be done with academic coaching.
Academic coaching is a process wherein a learner meets regularly with a faculty member to create goals, develop learning strategies and further develop professional identity. The goals should be consistent with the S.M.A.R.T format: specific, measurable, attainable, relevant and timely. Coaching will allow the learner to reflect and develop SMART goals. Once these goals have been created, FOAM and online resources can be used for regulatory mechanisms and regulatory appraisals.
Coaching can also guide the learner’s selected resources. For example, as a novice learner, Melissa may not know which resources to use to further her learning. Her coach can provide her with a list of relevant resources that align with her level of training. She will continue to meet with her coach and appraise her progress. As she successfully achieves her goals, she and her coach can gradually increase the complexity of her learning goals and her coach can provide more advanced FOAM resources.
Other examples of where this theory might apply
The clinical setting is a new frontier for many medical students and residents as they transition from tests to clinical performance. Those who came from a problem-based learning curriculum have been shown to use more self-regulated learning skills in their clinical performance.8
It is essential to stress that self-regulated learning is not an entirely learner independent process. This learning theory requires an instructor to help build foundational elements required for success.
Novices and experts view their learning in different ways. It is more difficult for novices than experts to engage in self-regulated learning because novices are more reliant on external feedback and direction at the beginning of their training.7 Self-regulated learning may be harder to develop in interns as opposed to senior residents.
This can be overcome with appropriate coaching and guidance. With appropriate guidance, a learner can set goals that are appropriate to his/her level of training. Educating the learner about the different regulatory mechanisms will assist them with goal achievement. Using an inquiry and advocacy framework will assist the learner in developing the skills of self reflection that are required for regulatory appraisal.
Melissa is an emergency medicine intern struggling to achieve her goal of becoming a good doctor. She is smart and motivated and recognizes that she needs to specify exactly what she means by becoming a good doctor. Her residency director introduces her to the educational theory of self-regulated learning in an effort to help Melissa achieve her professional goals.
Together, Melissa and her residency director develop an action plan focusing on three main academic areas: medical knowledge, patient care, and professionalism. Melissa develops a self-study plan composed of peer-reviewed FOAM resources and weekly question bank expectations. Self-study sessions take place during protected time in the hospital library to reduce distractions and include a mechanism for regular performance monitoring by her residency director.
Help seeking, motivation, planning, persistence, goal setting, and environmental structuring are all key elements of the self-regulated learning strategy. Baked into Melissa’s action plan are self-regulatory appraisals such as scheduled performance monitoring by her residency director. To further enhance her learning, Melissa also chooses to include regular self-evaluation via personal journaling, social media posting, and self-reflection.
Fast forward just a few months later and Melissa is excelling in her intern year. Her weekly quiz score leads her class. Her shift cards continue to rack up positive comments on patient care and professionalism. Self-regulated learning has made a real difference in Melissa’s development and success. As she gains more experience and insight, she will be able to independently set new goals, develop plans, determine progress, and titrate adjustments in her learning.
Annotated Bibliography
1. Sitzmann T, Ely K. A Meta-Analysis of Self-Regulated Learning in Work-Related Training and Educational Attainment: What We Know and Where We Need to Go. Psychological Bulletin. 2011;137(3):421-442.
This paper provides an overview of our current understanding of self-regulated learning and cites important research studies in the field.
2. Zimmerman, Barry J (1989). “A social cognitive view of self-regulated academic learning”. Journal of Educational Psychology. 81 (3): 329–339.
An early originator of self-regulated learning, Zimmerman introduces the self regulatory processes of learners that is central to the theory.
3. Cho, K. K., Marjadi, B., Langendyk, V., & Hu, W. (2017). The self-regulated learning of medical students in the clinical environment — a scoping review. BMC Medical Education, 17(1), 112.
This paper reviewed literature specifically focused on self-regulated learning in medical students adapting to the clinical environment. It identifies patterns in their self-regulated learning during different stages of their education.
10
Authors: Sugeet Jagpal, MD; Leon Melnitsky, DO; Sam Zidovetzki, MD, MPH
Editor: Anne Messman, MD
Irena, a junior faculty member at a medical school, is asked to consult on the development of a new medical school in her state. In particular, she is asked to comment on what should be taken into account in the admissions process. Irena remembers feeling quite confused by the components of the application process, and wonders if she could possibly suggest new angles that would make it easier for future applicants to apply to medical school. Excited about the prospect of being able to think through this de novo, Irena accepts the consulting offer.
As she reflects, negative memories of the application process come flooding back. She recalls having a letter of recommendation uploaded late, and the sheer panic that she felt at the time. She wondered back then, and still wonders to this day, if that missing letter of recommendation would have cost her her medical career. She also remembers working for days on her personal statement, only to find time and time again that interviewers had not taken the time to read it. One interviewer even told her that he did not look at personal statements prior to meeting the applicant – he trusted his ability to assess the applicants himself. He mentioned that in most cases he did not trust their ability to self report.
In addition, Irena was a biology major in college, and seriously thought about adding a minor in the liberal arts to make her application more well rounded for medical school. The added credits would have cost her additional money, and she chose against this as a preparatory course for the MCAT had already depleted her bank account. She ended up doing quite well on the MCAT, but would the money have been better spent on the minor in liberal arts? Would either of those have predicted success in medical school or a medical career?
Irena sincerely hopes that she will be able to suggest an admissions process that will allow medical schools to select excellent candidates AND prevent unnecessary angst in thousands of college students. She enthusiastically dives into the data behind the admissions process. She is pleasantly surprised to learn that this is a debated topic, and her concerns have been echoed by others. She zeroes in on Siu and Reiter’s TAU approach, drawn to their separation of the cognitive and non-cognitive domains of the admissions process.
Overview
The TAU approach to non-cognitive evaluation provides guidance to medical school admissions committees on predictive validity of assessment tools currently used for medical school admissions that describes three main principles.
T: Trust no one: Applicants are not trustworthy because the stakes are too high.
A: Avoid self-reporting: The weaker applicants are the worst self-assessors.
U: Use repeated measures: A single medical school interview is not reliable. It is recommended to implement a repeated measures approach to the selection process.
Main Originators of the Theory
Eric Siu & Harold I. Reiter
In the highly competitive market of medical school applicants, it is essential for the admissions committee to use reliable and valid selection tools. Most applicants to medical school are highly motivated individuals who will stop at very little in order to gain acceptance. Currently there are multiple tools available at the disposal of the medical school faculty. Applicants’ grade point average, Medical College Admissions Test score and the multiple mini-interview are among the most practically relevant and statistically significant in correlation to medical school performance.
The TAU perspective recommends having little faith in the validity of the current application process. In particular the “Trust no-one” approach is suggested when it comes to evaluating an applicant’s references, file reviewers or interviewers.
The applicants’ inability to objectively self report is highlighted in this paper. It is unreasonable to expect medical school candidates under tremendous pressure to honestly and reliably self-assess on the application. Using repeated measures to judge the validity of the interview process is deemed highly valuable. For example, multiple interviews are recommended instead of the single interaction in order to effectively predict candidates’ potential performance.
Letters of reference are a common part of an application, both for medical school and residency programs. Letters have been criticized as having poor predictive ability and poor inter-rater reliability.1 Since the TAU approach was published, a trend toward standardized letters of evaluation (SLOEs) has emerged in many medical schools. The SLOE allows for a more objective measurement and is not just a personal narrative, which was the primary mode of assessment in previous letters of reference.4 In addition to the narrative portion, a typical SLOE will contain seven competency-focused questions which require the evaluator to rank the applicant in one of several tiers.4 This ranking is to be done by multiple evaluators relative to the applicants’ peers which brings the SLOE well within the TAU framework of repeated measurements.
Scholarly activity in the form of publications and presentations has also been cited as important in the application process. A survey of Emergency Medicine Residency Directors listed scholarly activity as being an important factor in assessing an applicant.5 Other specialties such as general surgery and orthopedics have also had scholarly activity mentioned as an important component of an application.6 Scholarly activity can be assessed in an objective way with different weight being given to the strength of the study, publication or presentation in which the applicant participated. If objective criteria are used, scholarly activity can be used quantitatively to add to the global assessment of the applicant. This quantitative measurement fits with the TAU framework by avoiding self report.
The TAU frameworks are becoming more important as an increasing number of applications to health professions are non-traditional, providing significant diversity in the components of the application. This has increased the difficulty of comparing applications relative to each other. Using the TAU approach for admissions allows admissions committees to appreciate the uniqueness of each individual application without compromising the validity of predicting future success.
The TAU approach has far reaching applications to academic assessments beyond the application process itself. Clinical evaluations of residents and faculty are important indicators of performance and similarly should avoid self report. Classically Emergency Medicine resident assessment is done with one-on-one direct observation.7 This method of assessment is currently limited by evaluator bias and subjectivity. Although there are attempts to decrease this objectivity via interventions such as multiple choice testing or OSCEs, these are not repeated often enough in most training programs to be reliable.
Increasingly, evaluations of residents are milestone based, providing a framework for all faculty to assess residents objectively. These competency based evaluations are completed on a more frequent basis, and compared to other residents within the same program and across other programs to give a more accurate assessment of a residents’ performance.7 This is more consistent with the TAU approach.
Early career faculty new to their role would also benefit from a TAU approach to assessment of their administrative skills, teaching skills, bedside diagnostic acumen, and other roles they have been assigned. Colleagues of new faculty, support staff, and trainees should assess early faculty in several standardized parameters including teaching ability and bedside clinical skills. Those in existing administrative leadership roles should also give feedback to early faculty on their leadership skills and organizational abilities, instead of relying on their self assessment of these abilities. The principle of using objective data as part of a TAU approach at assessment is applicable to many clinical and educational realms.
The TAU approach has limitations as it allows for the possibility that future generations of applicants will go as far as modifying their applications solely in order to increase chances of admission thereby “cheating the system”. The “trust no one” theory can be interpreted as disrespectful and demeaning to the applicants and those that spend a significant amount of time writing required reference letters and various evaluations.
The TAU approach relies heavily on the MCAT as a predictor of success in medical school. It should be noted that in recent years, MCAT consulting and coaching has become increasingly popular. Those that can afford to pay $200/hour for a professional MCAT coach will have a higher chance at a better score, without having a higher chance of success in medical school itself. This also inherently increases the inequity of the admission process itself.
As far as mini interviews and use of “repeated measures,” there is a gray zone of uncertainty particularly when it comes to how defining how many mini interviews are required in order to conduct a reliable interview process. There is also no clear definition offered of the exact number of so called “repeated measures” regarding the number of interviewers that would satisfy criteria for multiple evaluations as suggested by the Siu and Reiter approach.
After a deep dive into the TAU approach, Irena submits her report to the medical school admissions committee. She recommends that they focus on the candidates’ GPAs, MCAT, and also rely on multiple mini interviews. She also recommends a de-emphasis on subjective measures such as personal statements and letters of reference. Given the higher likelihood of a better matched candidate with repeated measurements, she recommends scheduling multiple mini interviews for each potential candidate. She does clearly state in her report that the committee should look at all subjective data with caution.
She goes on to suggest an ideal interview process would involve initial screening of applications based on objective measurements such as GPA and MCAT scores. This would be followed by an interview day that involved multiple mini interviews, with only a brief review of personal statements and letters of recommendation as these were least likely to correlate with success.
Irena strongly suggests that in order to be as objective as possible, the medical school should undertake a training process for their interviewers as well as the admissions committee. By having people meet and determine beforehand what to look for in a letter of reference, for example, there would be an opportunity to create repeatable measurements to create some objectivity in this data. Another example would be to determine how to quantify scholarly activity – this would allow the committee to speak more objectively about the candidates, in line with the TAU approach. She suggests a debriefing after the admissions process so that all of those involved in the process can give and receive feedback, allowing the interviewers and committee to function as a team and to become a reliable resource for each other in the future.
In addition, she suggests that they track their enrolled students and adjust their admission screening process accordingly. By having an iterative process, she expects that they will be able to calibrate their admissions process with time and increase their satisfaction with their medical school class. In an ideal world, they would be able to track their admissions process to success in medical school and then success in the graduate medical education world, allowing them to fulfill their medical school’s mission. If a deficiency or need was identified, for example, in the residency milestones of their trainees they would be able to incorporate that both in their medical school curriculum as well as calibrate, if needed, their admissions process. This would be a very valuable resource for the medical school.
The admissions committee is grateful for Irena’s report. They inform her that they will be asking for her help moving forward as they calibrate their process.
Annotated Bibliography
1. Siu, E. and Reiter, H. (2009). Overview: what’s worked and what hasn’t as a guide towards predictive admissions tool development. Advances in Health Sciences Education, 14(5), pp.759-775.
This paper explains the TAU approach, stating tools that show predictive validity of future performance (such as the MCAT and multiple mini-interview) are perhaps more useful to the medical school admissions process than the tools that do not show validity (such as personal statement and letters of reference). This paper allows the reader to focus on each component of the admissions process individually.
2. de Visser, M., Fluit, C., Cohen-Schotanus, J. and Laan, R. (2017). The effects of a non-cognitive versus cognitive admission procedure within cohorts in one medical school. Advances in Health Sciences Education, 23(1), pp.187-200.
de Visser et al. 2017 discuss two different procedures for medical school admission (cognitive vs. noncognitive) and try to correlate them to outcomes in medical school completion. The cognitive procedure relied on scores on testing modalities, and the noncognitive procedure relied on noncognitive skills such as behavioral interviews. In their study, they used an algorithm to automate selective into medical school in two arms (cognitive procedure vs. noncognitive procedure) and compared students in each arm for dropout rates, grade in nursing attachment, and practical clinical course in year 3, along with a few other measurements. They demonstrated that students selected through cognitive procedures were less likely to drop out, and that students selected through the non-cognitive procedure had higher grades in nursing attachment and practical clinical course in year 3. They suggest that in order to avoid the drop out of potentially good clinical candidates early in the curriculum that selection at each medical school should resemble the early medical school curriculum.
3. de Visser, M., Fluit, C., Fransen, J., Latijnhouwers, M., Cohen-Schotanus, J. and Laan, R. (2016). The effect of curriculum sample selection for medical school. Advances in Health Sciences Education, 22(1), pp.43-56.
de Visser et al. 2016 describe using a selection process for medical school in which applicants were tested on tasks (such as taking online exams) that resembled early medical school. They discuss that they designed this to select applicants that would do well in their curriculum, and not necessarily the best doctors. They compared students selected in this manner to students selected via a lottery system. The selected students performed better, but the study did not follow long term outcomes so the long term effect is unclear.
1